Internal Medicine Chronic Obstructive Pulmonary Disease Case File
Eugene C. Toy, MD, Gabriel M. Aisenberg, MD
Case 15
A 58-year-old man comes to your office because of shortness of breath. He has experienced mild dyspnea on exertion for a few years, but more recently he has noted worsening shortness of breath with minimal exercise and the onset of dyspnea at rest. He has difficulty reclining; as a result, he spends the night sitting up in a chair trying to sleep. He reports a cough with production of yellowishbrown sputum every morning throughout the year. He denies chest pain, fever, chills, or lower extremity edema. He has smoked about two packs of cigarettes per day since age 15. He does not drink alcohol. A few months ago, the patient went to an urgent care clinic for evaluation of his symptoms, and he received a prescription for some inhalers, the names of which he does not remember. He was also told to find a primary care provider for further evaluation. On physical examination, his blood pressure is 135/85 mm Hg, heart rate is 96 beats per minute (bpm), respiratory rate is 28 breaths/min, and temperature is 97.6 °F. He is sitting in a chair, leaning forward, with his arms braced on his knees. He appears uncomfortable, with labored respirations and cyanotic lips. He is using accessory muscles of respiration, and chest examination reveals wheezes and rhonchi bilaterally, but no crackles are noted. The anteroposterior (AP) diameter of the chest wall appears increased, and he has inward movement of the lower rib cage with inspiration. Cardiovascular examination reveals distant heart sounds but with a regular rate and rhythm, and his jugular venous pressure (JVP) is normal. His extremities show no cyanosis, edema, or clubbing.
▶ What is the most likely diagnosis?
▶ What are the next best diagnostic tests?
▶ What is the best initial treatment?
ANSWERS TO CASE 15:
Chronic Obstructive Pulmonary Disease
Summary: A 58-year-old man presents with
- Worsening shortness of breath with minimal exercise and the onset of dyspnea at rest with difficulty reclining
- History of smoking two packs of cigarettes per day since age 15
- Reports of a productive cough with yellowish-brown sputum every morning throughout the year
- Sitting in a characteristic “tripod” position to facilitate use of accessory muscles of respiration
- The appearance of an airway obstruction with respiratory distress, lower chest retractions, and bilateral wheezes and rhonchi
- Perioral cyanosis suggesting hypoxemia
- An increased appearance of the anteroposterior diameter of the chest wall
Most likely diagnosis: Chronic obstructive pulmonary disease (COPD) with acute exacerbation.
Next diagnostic steps: Arterial blood gas (ABG) to assess oxygenation and acid-base status and chest x-ray.
Best initial treatment: Oxygen by nasal cannula, followed closely by bronchodilators and steroids for airway inflammation.
- Define chronic bronchitis, COPD, and emphysema. (EPA 1, 2)
- Describe spirometry and flow-volume loops and their value for the diagnosis and management of obstructive and restrictive lung diseases. (EPA 3)
- Describe the treatment of stable COPD, as well as management of acute exacerbations, including the indications for mechanical ventilation. (EPA 4, 10, 12)
Considerations
This 58-year-old, long-time smoker likely has COPD. He is now in respiratory distress with labored respirations, cyanosis, and wheezing. The urgent issue is his current respiratory status. Rapid clinical assessment is critical in case this patient is headed toward respiratory failure, perhaps necessitating endotracheal intubation and mechanical ventilation. An ABG will quickly provide information regarding the adequacy of oxygenation status (Pao2) and ventilation (Paco2). A chest x-ray will determine the underlying status of the lung parenchyma and whether a trigger for the current situation can be identified.
APPROACH TO:
Chronic Obstructive Pulmonary Disease
DEFINITIONS
CHRONIC BRONCHITIS: COPD component that is diagnosed clinically and is characterized by excessive secretion of bronchial mucus and productive cough for 3 months or more in at least 2 consecutive years in the absence of any other disease that might account for this symptom.
CHRONIC OBSTRUCTIVE PULMONARY DISEASE (COPD): Chronic airflow obstruction caused by chronic bronchitis or emphysema. COPD is a preventable and treatable disease characterized by persistent airflow limitation that is usually progressive and associated with enhanced chronic inflammatory response in the lungs to noxious particles and gases. Diagnosis in the right clinical setting is usually supported by FEV1/FVC ratio less than 0.7. Severity of COPD on spirometry is based on the level of FEV1/FVC ratio compared to the predicted value. The severity of airflow limitation can be classified based on postbronchodilator FEV1 (Table 15–1).
EMPHYSEMA: COPD component that inferred clinically, and is diagnosed pathologically with abnormal, permanent enlargement of air spaces distal to the terminal bronchioles, with destruction of their walls and without obvious fibrosis.
FEV1/FVC: Ratio involving volume expired in the first second and the vital capacity (VC) in maximal effort, reduced in obstructive lung disease.
FORCED EXPIRATORY VOLUME IN 1 SECOND (FEV1): Volume of air expired in the first second during maximal expiratory effort. FEV1 is reduced in both obstructive lung disease (increased airway resistance) and restrictive lung disease (low VC).
FORCED VITAL CAPACITY (FVC): Total volume of air expired after full inspiration. FVC is reduced in restrictive lung disease.
OBSTRUCTIVE LUNG DISEASE: Chronic pulmonary disorder that is characterized by a disproportional decrease in maximal airflow from the lung in relation to maximal volume that can be displaced from the lung. Typically, FEV1 will be decreased relative to FVC; therefore, the FEV1/FVC will be decreased. The most common types of obstructive lung disease are asthma and COPD.

PULMONARY FUNCTION TEST (PFT): Complete PFTs comprise respiratory tests of spirometry, lung volumes, and diffusion.
RESTRICTIVE LUNG DISEASE: Chronic pulmonary disorder characterized by low lung volumes. Can be due to intrinsic factors, such as changes in the lung parenchyma, or extrinsic factors, such as alterations of the chest wall, pleura, or respiratory muscles. Typically, the FVC and FEV1 are reduced, but the FEV1/FVC is normal. The diagnosis is best made by a reduced total lung capacity (TLC).
SPIROMETRY: Method of evaluating respiratory flow volumes and flow rates to assess pulmonary function.
CLINICAL APPROACH
Pathophysiology
The most common etiology for COPD is inhalation injury, specifically cigarette smoking. Another important cause is alpha-1 antitrypsin deficiency, which is hereditary; pulmonary disease may become evident by age 40 and may occur without cough or smoking history. Therapy by replacement of alpha-1 antitrypsin enzyme is available. Characteristically, patients with COPD present with progressively worsening dyspnea (first on exertion, then with activity, then at rest). Patients may vary in appearance from a “blue bloater” (chronic bronchitis, overweight, edematous, cyanotic) to a “pink puffer” (emphysema, thin, ruddy cheeks).
Arterial blood gases often are normal in the early phase of the disease; however, in more advanced disease, there is evidence of hypoxemia and hypercapnia, often with a chronic compensated respiratory acidosis as a consequence of CO2 retention. Such chronic stable patients may have a Pao2 near 50 mm Hg and a Paco2 near 50 mm Hg, but a near-normal pH (the “50-50” club). During an acute exacerbation, more severe hypoxemia or hypercapnia, or respiratory acidosis noted on ABG, may be an indication of impending respiratory failure and need for ventilatory support. Given an appropriate clinical context, general indications for measuring ABGs include low oxygen saturation on pulse oximetry (< 92%), depressed level of consciousness, acute exacerbation, or assessment of hypercapnia in at-risk patients 30 to 60 minutes after supplemental oxygen is initiated.
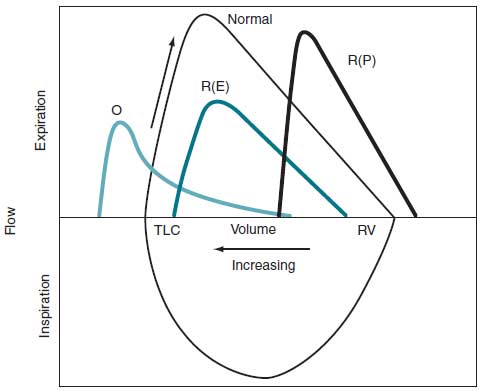
Spirometry is the most basic, inexpensive, widely valuable PFT to diagnose pulmonary diseases (Figure 15–1). Spirometric tracings of forced expiration (Figure 15–2) and flow-volume loops (Figure 15–3) help to identify the type of lung disease (obstructive vs restrictive), as well as potential reversibility of airflow obstruction. Restrictive lung diseases tend to have lower lung volumes (decreased TLC and VC), whereas obstructive diseases have larger lung volumes (TLC normal or increased) with decreased expiratory flow rates (reduced FEV1 < 80% expected, and FEV1/FVC < 0.7). Specific parameters help to classify the type and degree of lung dysfunction (Table 15–2). Reduced FEV1/FVC with minimal response to bronchodilators is the hallmark of COPD.
Figure 15–1. Expiratory flow-volume loops of normal, obstructive, and restrictive lung disease.
Treatment
Management of severe COPD exacerbations focuses simultaneously on relieving airway obstruction and correcting life-threatening abnormalities of gas exchange. Bronchodilators (beta-agonist and anticholinergic agents) are administered via handheld nebulizers; systemic glucocorticoids accelerate the rate of improvement in lung function among these patients. Antibiotics should be given if there is suspicion of a respiratory infection. Controlled oxygen administration with nasal oxygen at low flows or oxygen with Venturi masks will correct hypoxemia without causing severe hypercapnia. It is prudent to watch for CO2 retention and consequent apnea in these patients due to the effects of oxygen causing increased V/Q mismatch, loss of

Figure 15–2. Spirographic tracing of forced expiration, comparing normal tracing (A) with that of patients with obstructive (B) and restrictive (C) lung disease. Calculations of FVC, FEV1, and forced expiratory flow (FEF) (25%-75%) are shown for the normal tracing. The curves are positioned to show the relative starting lung volumes in each of these different conditions. Lung volumes increase to the left on the horizontal axis. FEV1, forced expiratory volume in first second; FVC, forced vital capacity; VC, vital capacity. (Reproduced with permission, from Braunwald E, Fauci AS, Kasper KL, et al. Harrison’s Principles of Internal Medicine. 17th ed. 2008. Copyright © McGraw Hill LLC. All rights reserved.)
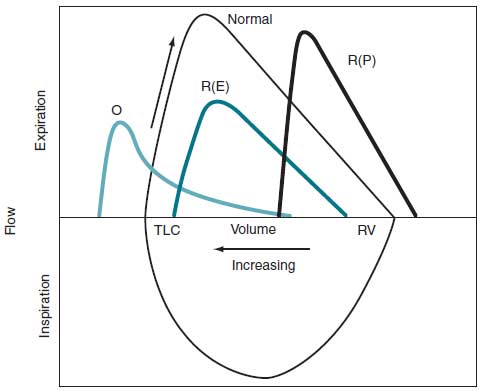
Figure 15–3. Flow-volume curves showing forced inspiratory and expiratory volumes in lung disease: O, obstructive lung disease (eg, COPD); R(P), parenchymal restrictive disease (eg, pulmonary fibrosis); R(E), extraparenchymal restrictive disease (eg, chest wall deformity) with limitation of both inspiration and expiration. Lung volumes increase to the left on the horizontal axis. TLC, total lung capacity. (Reproduced with permission, from Braunwald E, Fauci AS, Kasper KL, et al. Harrison’s Principles of Internal Medicine. 17th ed. 2008. Copyright © McGraw Hill LLC. All rights reserved.)
hypoxemic respiratory drive, and Haldane effect. The Haldane effect describes how the binding of O2 to hemoglobin reduces hemoglobin CO2 affinity. Deoxygenation of blood increases the ability of hemoglobin to carry CO2, whereas oxygenated blood has reduced capacity for CO2.
Positive pressure mask ventilation, such as continuous positive airway pressure (CPAP) or bilevel positive airway pressure (BiPAP), offers an alternative to
Abbreviations: ARDS, acute respiratory distress syndrome; FEV1, forced expiratory volume in 1 second; FVC, forced vital capacity; TLC, total lung capacity; VC, vital capacity.
intubation and mechanical ventilation in the treatment of cooperative patients with an acute exacerbation of COPD and severe hypercapnia. Signs of acute respiratory failure include tachypnea (respiratory rate > 40 breaths/min), inability to speak because of dyspnea, accessory muscle use with fatigue despite maximal therapy, confusion, restlessness, agitation, lethargy, a rising Paco2 level, and extreme hypoxemia. Acute respiratory failure is generally treated with endotracheal intubation and mechanical ventilatory support to correct the gas exchange disorders. Complications of mechanical ventilation include difficulty in extubation, ventilator-associated pneumonia, and pneumothorax.
Other therapies such as inhaled bronchodilators (beta-agonists and/or anticholinergics) or inhaled glucocorticoids are used for symptomatic relief and to reduce the frequency of exacerbations. Therapeutic recommendations are based on the disease stage, per the Global Initiative for Chronic Obstructive Lung Disease (GOLD) guidelines (Table 15–3).
Abbreviations: FEV1, forced expiratory volume in 1 second; FVC, forced vital capacity.
Complications
Long-term complications of COPD from hypoxemia can cause pulmonary hypertension, secondary erythrocytosis, exercise limitation, and impaired mental functioning. For patients with COPD who are stable, only smoking cessation, supplemental oxygen therapy for patients with chronic hypoxemia, and lung volume reduction surgery in selected patients have been shown to alter the natural history of the disease and provide a reduction in mortality. Patients with resting hypoxemia (Pao2 < 55 mm Hg or arterial oxygen saturation [Sao2arterial oxygen saturation] < 88%) generally benefit from home oxygen therapy, which must be utilized at least 18 h/d.
CASE CORRELATION
- See also Case 14 (Pulmonary Embolism), Case 16 (Chronic Cough/Asthma), Case 17 (Pleural Effusion, Parapneumonic), and Case 19 (Community-Acquired Pneumonia).
COMPREHENSION QUESTIONS
15.1 A 65-year-old man is being seen in the office for shortness of breath of 1 day’s duration. He has smoked 1.5 packs of cigarettes per day for 35 years. On examination, he is cachectic and breathes with pursed lips. His chest is barrel-shaped, and the AP diameter is enlarged. Which of the following is the most likely physical examination finding in this patient?
A. Diffuse expiratory wheezing
B. Clubbing of the fingers
C. Bibasilar inspiratory crackles with increased JVP
D. Inspiratory stridor
E. Third heart sound
15.2 A 56-year-old woman is being seen in the office for a history of shortness of breath that has worsened over the past month. She admits to a 60 pack-year smoking history. She complains of fatigue and dyspnea with minimal exertion and a productive cough each morning. Pulmonary function testing is ordered. Which of the following is the most likely finding in this patient?
A. Higher diffusing capacity of lung for carbon monoxide (DLCO)
B. Decreased residual volume
C. Normal FEV1
D. Decreased FEV1/FVC
E. Decreased FVC
15.3 Which of the following therapies is most likely to provide the greatest benefit to a patient with chronic stable emphysema and a resting oxygen saturation of 86%?
A. Inhaled tiotropium daily
B. Inhaled albuterol as needed
C. Oral prednisone daily
D. Supplemental oxygen used at night
E. Supplemental oxygen used continuously
ANSWERS
15.1 A. COPD is characterized by chronic airway obstruction, with most airflow resistance occurring in small airways of the lower respiratory tract, producing expiratory wheezing. Inspiratory stridor (answer D) would occur with upper airway, usually extrathoracic, obstruction. Clubbing (answer B) is not generally a feature of COPD unless there is long-standing cyanosis and should prompt investigation for another disease process, such as a bronchogenic carcinoma. Crackles and elevated JVP (answer C), as well as an S3 (answer E), are signs of heart failure.
15.2 D. This patient likely has COPD, based on the smoking history and symptoms. A decrease in the FEV1/FVC ratio is the hallmark of airflow obstruction. The FEV1 is decreased in obstructive and restrictive lung disease, and therefore answer C (normal FEV1) is incorrect. The diffusing capacity is typically decreased (answer A) in COPD as well as intrinsic restrictive lung disease. The DLCO indicates the adequacy of the alveolar-capillary membrane; the residual volume is the volume of air remaining in the lungs after a maximal expiratory effort and is usually increased (answer B) in COPD due to air trapping. The FVC is typically normal to increased with COPD, which is why answer E is incorrect.
15.3 E. For patients with chronic hypoxemia, supplemental oxygen has a significant impact on mortality, with a greater benefit with continuous usage rather than intermittent or nocturnal-only usage (answer D). Bronchodilators such as tiotropium (answer A) and albuterol (answer B) improve symptoms and FEV1 but offer no mortality benefit. Chronic use of oral corticosteroids (answer C) should be avoided because of unfavorable side effects, such as osteoporosis, glucose intolerance, and gastrointestinal (GI) side effects.
CLINICAL PEARLS
▶ Patients with obstructive lung disease have airflow limitation on expira-tion (reduced FEV1/FVC), whereas patients with restrictive lung disease have difficulty in expanding their lung volumes in response to exercise (reduced TLC).
▶ The mainstay for treatment of COPD exacerbations includes bronchodi-lators, oxygen, and glucocorticoids, as well as antibiotics if infection is suspected.
▶ Controlled supplemental oxygen along with positive pressure mask ven-tilation (BiPAP) may prevent respiratory failure requiring endotracheal intubation.
▶ Smoking cessation and supplemental oxygen to treat chronic hypoxemia are the only medical therapies shown to decrease mortality among per-sons with COPD.
▶ In both obstructive and restrictive lung disease, the FEV1 is decreased; the FEV1/FVC is decreased in obstructive processes and normal in restric-tive processes.
▶ The hallmark of restrictive lung disease is decreased lung capacity, particularly the TLC but also the VC.
REFERENCES
Han ML, Dransfield MT, Martinez FJ. Chronic obstructive pulmonary disease: Definition, clinical manifestations, diagnosis, and staging. Post TW, ed. UpToDate. Waltham, MA: UpToDate Inc.
https://www.uptodate.com/contents/chronic-obstructive-pulmonary-disease-definition-clinical-manifestations-diagnosis-and-staging. Accessed June 16, 2019.
Pauwels RA, Buist S, Calverley PMA, et al. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease. NHLBI/WHO Global Initiative for Chronic Obstructive Lung Disease (GOLD) workshop summary. Am J Respir Crit Care Med. 2001;163:1256-1276.
Reilly JJ, Silverman EK, Shapiro SD. Chronic obstructive pulmonary disease. In: Jameson JL, Fauci AS,
Kasper DL, et al, eds. Harrison’s Principles of Internal Medicine. 20th ed. New York, NY: McGraw Hill; 2018:1380-1388.
Sutherland ER, Chemiak RM. Management of chronic obstructive pulmonary disease. N Engl J Med. 2004;350:2689-2697.
Weinberger SE, Rosen IM. Disturbances of respiratory function. In: Longo DL, Fauci AS, Kasper DL, et al, eds. Harrison’s Principles of Internal Medicine. 20th ed. New York, NY: McGraw Hill; 2018:1380-1388.






0 comments:
Post a Comment
Note: Only a member of this blog may post a comment.