Trigger Finger Case File
Eugene C. Toy, MD, Andrew J. Rosenbaum, MD, Timothy T. Roberts, MD, Joshua S. Dines, MD
CASE 32
A 60-year-old right-hand dominant woman presents complaining of 12 weeks of right ring finger pain. She is an avid gardener but denies any injury. She notes a clicking sensation when she moves her finger. She occasionally experiences the finger “getting stuck” when she bends it and she has to use her other hand to force the finger back into extension. She reports minimal pain at rest. The pain does not awaken her at night, but she does note ring finger stiffness in the morning. She denies swelling or redness. She has tried resting and limiting her gardening, and she has been taking ibuprofen. Her medical history includes diabetes. On examination, the skin is intact and appears normal. There is no atrophy, swelling, ecchymosis, or erythema. She has a full range of passive and active motion of her fingers and wrist. There is tenderness over the palmar aspect of the ring finger metacarpophalangeal (MCP) joint and palpable popping with active finger flexion and extension. Strength is 5/5 in finger flexion, extension, and abduction/adduction. Sensation is intact to light touch. She has 2+ pulses and capillary refill is less than 2 seconds. Compression testing at the carpal tunnel is negative, as is Phalen and Tinel testing. Hand radiographs show intact joint spaces and normal alignment.
► What is the most likely diagnosis?
► What is the next diagnostic step?
► What is the next step in therapy?
ANSWER TO CASE 32:
Trigger Finger
Summary: A 60-year-old diabetic woman presents to the office with 6 weeks of right ring finger pain, popping, and locking with no history of injury. There is tenderness to palpation over the flexor tendons overlying the MCP joint and palpable triggering. There is full range of motion and good strength.
- Most likely diagnosis: Trigger finger.
- Next diagnostic step: Physical exam is usually sufficient to diagnose this condition. Further confirmation may be achieved with an injection of local anesthetic into the flexor tendon sheath. This results in a temporary resolution of pain so that triggering, if present, can be readily elicited.
- Next step in therapy: This patient has a 12-week history of symptoms and has not seen improvement after rest, activity modification, and NSAIDs. The next step is steroid injection into the flexor tendon sheath.
ANALYSIS
Objectives
- Understand the pathoanatomy of trigger finger.
- Appreciate the functions of the flexor tendons and the flexor pulley system and how they relate to trigger finger.
- Be familiar with the treatment options for trigger finger.
Considerations
This 60-year-old woman with finger pain and popping has tendon entrapment, also known as trigger finger. The diagnosis can generally be made with a thorough history and physical examination. It is important to rule out more serious causes for finger pain, including infection or fracture. Infection would have associated swelling, erythema, and possibly constitutional symptoms such as fever and chills. Fractures result from an injury and initially will have swelling and ecchymosis. These conditions can easily be ruled out in this case by the history and exam. If doubt exists, plain radiographs can be used to rule out fracture, arthritis, or underlying bony deformity. Other common conditions should also be ruled out, including arthritis and carpal tunnel syndrome. Arthritis is a common cause of joint pain and stiffness in the hand. Examination will reveal tenderness over the joint. In this patient’s case, the tenderness is over the palmar aspect of the MCP joint. Anatomically, this region of the joint is covered by the flexor tendons and pulley system. The radial and ulnar sides of the MCP joint are more accessible to palpation and are nontender in this patient.
The severity of the mechanical symptoms in a patient with trigger finger should be determined. Early on, some patients may complain of pain alone, whereas in more advanced cases, patients may have significant popping and locking to the point that the finger becomes fixed in a flexed position. This can lead to permanent loss of motion in the finger if untreated.
APPROACH TO:
Trigger Finger
DEFINITIONS
TENOSYNOVIUM: Thin synovial lining surrounding tendons that provides lubricating fluid and nutrition to the tendons.
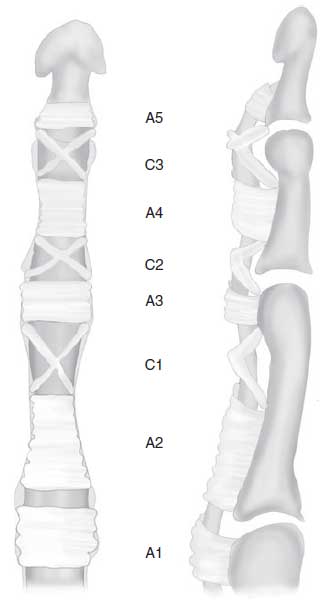
PULLEY: Fibrous sheath through which the flexor tendon glides. The flexor tendon sheath functions to improve mechanics and maintain the tendon against the metacarpal and phalanges. In each finger, there are 4 to 5 annular (circular) pulleys and 3 cruciate (crossing) pulleys that make up the tendon sheath ( Figure 32–1 ).
Figure 32–1. Finger flexor tendon pulley system. The pulleys are attached to the palmar surface of
each finger metacarpal (MC), proximal phalanx (PP), middle pharynx (MP), and distal pharynx (DP).
There are 5 annular pulleys, A1 through A5, and 3 cruciate pulleys (C1-3). Triggering occurs when
there is narrowing at the A1 pulley. (Reproduced, with permission, from Brunicardi FC, Andersen DK, Billiar TR, et al. Schwartz’s Principles of Surgery. 9th ed. New York, NY: McGraw-Hill; 2010:Fig. 44-4.)
TRIGGER FINGER (ie, tendon entrapment): Inflammation of the tenosynovium and narrowing of the first pulley, resulting in pain and popping with finger movement.
FINGER FLEXOR TENDONS: Each finger has 1 tendon from the flexor digitorum profundus, which attaches to the distal phalanx and flexes the distal interphalangeal joint (DIP), and 2 slips (derived from a single tendon) from the flexor digitorum superficialis (FDS), which attach to the middle phalanx and flex the proximal interphalangeal joint (PIP). The thumb pulley system contains the flexor pollicis longus and attaches to the distal phalanx, flexing the thumb interphalangeal joint.
CLINICAL APPROACH
Etiologies
Tendon entrapment can occur in any finger or the thumb. It is also common to see patients with multiple fingers affected. Trigger finger is most common in patients 55 to 60 years of age and is at least twice as common in women as in men. It is generally thought to be a degenerative condition resulting from long-term repetitive use of the hand, especially with repeated gripping or pinching. It is more commonly seen in the dominant hand. Systemic factors that can cause or exacerbate tendon entrapment include diabetes, gout, and rheumatoid arthritis.
The flexor tendons glide through a series of fibrous pulleys ( Figure 32–1 ) that make up the tendon sheath. The pulleys act to constrain the tendons against the bone. This increases the force transmission and allows tendon gliding with finger motion. There are 4 to 5 annular pulleys and 3 cruciate pulleys. The A2 and A4 pulleys are most critical for function. The first pulley (A1) may become narrowed over time, leading to tendon entrapment. The tendons are lined with a thin tenosynovium that provides lubrication and nutrition. With repetitive use of the hand, the tenosynovium may become inflamed, resulting in pain over the tendon aggravated by use (termed tenosynovitis ). As the condition worsens, degenerative changes in the fibrous pulley occur, resulting in thickening and inflammatory cell infiltration. As the A1 pulley becomes more hypertrophied, stenosis or narrowing occurs. This leads to a popping or catching sensation with finger flexion and extension as the tendon bunches up and gets stuck in the pulley.
Clinical Presentation
In the early stages of the condition, pain is the primary complaint. Pain is reported with activities that involve use of the hand, especially gripping or holding objects. Most patients report minimal pain at rest but may experience sharp pain with aggravating activities. As the condition worsens, popping begins to occur with active finger motion. The finger may begin to “catch” or temporarily get stuck and, in more advanced cases, may lock in a flexed position, requiring assistance to force the finger back in extension. Patients often complain of stiffness upon waking in the morning and may note that the finger is locked in flexion when they wake up. There is generally no swelling, numbness, or tingling. However, some patients can feel a bump or a nodule in the flexor tendons that is tender to the touch.
Physical examination usually confirms the diagnosis. The A1 pulley, which overlies the metacarpal head and can be felt as a bump at the base of each finger in the distal aspect of the palm, is palpated and is very tender to touch in the setting of trigger finger. There is generally no tenderness elsewhere. Next, range of motion should be examined and is usually normal. In severe cases with chronic locking, some patients may develop a flexion contracture where they cannot fully extend the finger. The examiner should then palpate over the A1 pulley while the patient actively flexes and extends the finger to check for popping. One may also note a nodularity in the tendon as it glides with finger motion. A complete examination of the hand and wrist should be performed to rule out other conditions.
Radiographs are routinely obtained to rule out other conditions including arthritis and fracture. There are no radiographic abnormalities associated with trigger finger. The diagnosis can be confirmed with an injection of local anesthetic into the flexor tendon sheath. This will result in complete pain resolution.
TREATMENT
Conservative treatment is effective in most patients with a trigger finger. In early cases with mild symptoms, simple activity modification, rest, and oral anti-inflammatories may be effective. With more significant pain and popping and in more chronic cases, the next step is usually a steroid injection into the flexor tendon sheath. Injections have been reported to result in complete symptom resolution in 57% of cases, but some patients may require more than one injection. Patients with systemic causes for trigger finger such as diabetes have worse results with conservative treatment, with success seen in less than 50%.
In cases that do not respond to conservative treatment, surgery is an option. This involves surgically dividing the A1 pulley to relieve the tendon entrapment. The A2 and other distal pulleys remain intact, and no function is compromised. The success rate of surgery is very high (> 90% by most reports).
COMPREHENSION QUESTIONS
32.1 A 55-year-old woman presents with sudden catching and locking of her ring finger when trying to extend it. She experiences severe pain and notes tenderness in her distal palm. You suspect that this is a trigger finger. What is the best test for confirming this diagnosis?
A. X-raysB. Computed tomography scanC. Magnetic resonance imagingD. Lidocaine injectionE. Ultrasound of the hand
32.2 A 45-year-old woman whom you have recently diagnosed with trigger finger asks you to explain in greater detail why her ring finger locks with flexion. Which of the following statements is most accurate regarding the mechanism for triggering?
A. Trigger finger is caused by entrapment of the flexor tendons at the level of the A1 pulley.B. The mechanism that causes the finger to trigger is unknown.C. Trigger finger is due to a vascular anomaly.D. Trigger finger is caused by a traumatic rupture of the A1 pulley.
32.3 A diabetic patient with a chronic trigger finger has locking of the finger with flexion and has failed 2 prior steroid injections. What is the most effective treatment option for this patient?
A. SurgeryB. Repeat steroid injectionC. Physical therapyD. Finger splintingE. Oral anti-inflammatories
ANSWERS
32.1 D. A lidocaine injection into the flexor tendon sheath resulting in complete pain relief confirms the diagnosis. However, history and physical exam are usually adequate for the diagnosis, and further confirmation is not required in most cases.
32.2 A. The flexor tendons glide through a series of fibrous pulleys that make up the tendon sheath. The first pulley (A1) may become narrowed over time, and as it becomes more hypertrophied, stenosis or narrowing occurs. This leads to a popping or catching sensation with finger flexion and extension as the tendon bunches up and gets stuck in the pulley.
32.3 A. This patient has failed 2 injections, and other conservative treatments are unlikely to be effective because of the associated diabetes. Surgical release of the A1 pulley has a success rate of greater than 90%.
CLINICAL PEARLS
|
► Trigger finger is caused by flexor tendon entrapment in a narrowed A1 pulley. ► Trigger finger usually responds to conservative treatment. ► A steroid injection into the tendon sheath is an effective treatment in most cases and usually should be attempted before considering surgery. ► Surgical release of the A1 pulley is very effective in most cases that do not respond to conservative treatment. |
REFERENCES
Fleisch SB, Spindler KP, Lee DH. Corticosteroid injections in the treatment of trigger finger: a level I and II systematic review. J Am Acad Orthop Surg. 2007;15:166-171.
Saldana MJ. Trigger digits: diagnosis and treatment. J Am Acad Orthop Surg. 2001;9:246-252.
Wolfe SW, et al. Green’s Operative Hand Surgery . 6th ed. Philadelphia: Elsevier; 2011:2071-2079.

0 comments:
Post a Comment
Note: Only a member of this blog may post a comment.