Lisfranc Injury Case File
Eugene C. Toy, MD, Andrew J. Rosenbaum, MD, Timothy T. Roberts, MD, Joshua S. Dines, MD
CASE 36
A 37-year-old man arrives in the emergency department after a motorcycle accident in which he hit a tree traveling at approximately 50 mph. He was helmeted and denies any loss of consciousness. His blood pressure is 130/80 mmHg, his heart rate is 90 beats/minute, and his temperature is 99°F. He complains of significant pain localized to his right foot. On physical exam of the right foot, the skin is found to be intact. However, there is significant swelling over the dorsum of the foot as well as plantar ecchymosis. His foot is tender, predominantly over the midfoot and forefoot. The patient will not move his toes secondary to pain. His sensation is grossly intact. The posterior tibial pulse is palpable, whereas the dorsalis pedis pulse is only appreciated with a Doppler probe. Capillary refill of the toes is brisk and less than 2 seconds. His pain does not worsen with passive dorsiflexion of the toes.
► What initial radiographic studies are most appropriate?
► What is the most likely diagnosis?
► Given the mechanism of injury, what other considerations must be taken before initiating appropriate treatment for the patient’s foot?
► How is this injury classified?
► What is the most appropriate treatment for this patient?
ANSWER TO CASE 36:
Lisfranc Injury
Summary: A 37-year-old man complains of severe right foot pain after a motorcycle accident in which he hit a tree at approximately 50 mph. On physical exam of his foot, diffuse tenderness and dorsal swelling are noted, as is medial plantar ecchymosis.
- Radiographs to order: Anteroposterior (AP), lateral, and 30-degree oblique views of the right foot.
- Most likely diagnosis: Tarsometatarsal joint complex injury, commonly referred to as a Lisfranc injury.
- Other considerations: Given the high-energy mechanism of injury, this patient must be managed with strict adherence to advanced trauma life support protocol. A complete trauma workup and evaluation should be performed before orthopaedic intervention for the left foot.
- Classification of Lisfranc injury: Although multiple classifications exist, none have been proven to be useful for determining treatment or prognosis. One commonly used descriptive classification describes homolateral, isolated, and divergent patterns.
- Treatment: Open-reduction internal fixation when soft tissue swelling subsides.
- Be familiar with the general presentation of a Lisfranc injury.
- Understand the workup and imaging studies required for diagnosis of a Lisfranc injury.
- Know the treatment options for and complications associated with Lisfranc injuries.
Considerations
This patient’s history and presentation are common for an injury to the tarsometatarsal (TMT) joint complex. The diffuse pain and swelling, specifically over the midfoot and forefoot, are consistent with a high-energy injury mechanism, such as a motorcycle accident, which is often associated with Lisfranc injuries. Additionally, the medial plantar ecchymosis is often thought to be pathognomonic for this injury. The absence of a palpable dorsalis pedis pulse is likely due to the soft tissue swelling over the dorsum of the foot, another common finding. Although the patient’s clinical picture is consistent with a Lisfranc injury, up to 20% of these initially go undiagnosed. The swelling is concerning, as compartment syndrome of the foot can be seen in association with injuries to the TMT joint complex. The practitioner must carefully and serially examine the patient in this setting and even consider measuring compartment pressures if they believe an acute compartment syndrome is present. The orthopaedic workup of this patient should also include imaging of the right foot, including AP, lateral, and oblique views. A secondary survey should also be performed to rule out additional musculoskeletal injuries requiring care. In the emergency department, this patient’s foot should be splinted, iced, and elevated to control swelling, as the timing of potential operative intervention is dependent on this. Soft tissue swelling can delay operative treatment of Lisfranc injuries by up to several weeks. In addition to an orthopaedic surgery consultation, this patient requires an evaluation by the trauma team; intracranial, thoracic, abdominal, and spine injuries can be present concurrently.
APPROACH TO:
Lisfranc Injuries
DEFINITIONS
JACQUES LISFRANC: A field surgeon in Napoleon’s army. He described an amputation involving the TMT joint due to a severe gangrene that developed when a soldier fell from a horse with his foot caught in a stirrup.
LISFRANC JOINT: This refers to the TMT joint complex, an osseous and capsule- ligamentous network that includes the 5 metatarsals (MTs), their articulations with the cuneiforms and cuboid, and the Lisfranc ligament, a strong interosseous attachment between the medial cuneiform and second MT.
LISFRANC INJURY: Refers to a spectrum of processes involving the TMT joint complex, including both fractures and dislocation. It does not delineate a specific injury.
HOMOLATERAL LISFRANC INJURY: All 5 metatarsals are displaced in the same direction.
ISOLATED LISFRANC INJURY: 1 or 2 metatarsals are displaced from the others.
DIVERGENT LISFRANC INJURY: The metatarsals are displaced in both the coronal and sagittal planes.
COMPARTMENT SYNDROME: A surgical emergency that occurs as a result of increased pressure within a muscle compartment, at times compromising blood flow and damaging nerves, muscle, and surrounding soft tissue structures. It is often encountered in the setting of trauma and extremity fractures. Although a clinical diagnosis, intracompartmental pressure measurements of greater than 30 mmHg or a less than 30-mmHg difference between the patient’s intracompartmental pressure and diastolic blood pressure are consistent with the diagnosis of compartment syndrome (see Case 13).
CLINICAL APPROACH
Anatomy
The Lisfranc joint divides the midfoot and the forefoot, forming an oblique line running from the lateral aspect of the proximal forefoot to the medial aspect of the distal forefoot. Bony elements provide the primary structural support to this articulation, with ligamentous contributions adding additional stability. The 3 medial MTs articulate with the 3 cuneiforms; the fourth and fifth MTs articulate with the cuboid. The middle cuneiform–second MT articulation forms the keystone of the arch, preventing mediolateral MT motion at the Lisfranc joint. This transverse arch also prevents plantar displacement of the 3 medial MTs. The most significant and strongest ligamentous structure is the oblique interosseous ligament, referred to as Lisfranc ligament. Originating on the lateral surface of the medial cuneiform, it passes in front of the intercuneiform ligament and ultimately inserts on the medial aspect of the second MT base near the plantar surface.
Mechanism
Direct and indirect injury patterns can damage the Lisfranc joint. Direct mechanisms, most commonly crush injuries, are due to high-energy blunt trauma to the dorsum of the foot. These often result in worse clinical outcome as compared with indirect types, secondary to the associated soft tissue trauma. The indirect mechanism usually involves axial loading of a plantarflexed foot, external rotation on a pronated forefoot, or an abduction stress to the midfoot. Indirect mechanisms are stratified into high-energy and low-energy subtypes. Motor vehicle accidents are the most common cause of high-energy Lisfranc injury. Low-energy injuries include those incurred during athletic competition. The fracture pattern and direction of dislocation in direct injuries are dependent on the force vector applied. Indirect injuries are more predictable and most commonly involve failure of the weaker dorsal TMT ligaments in tension with subsequent dorsal or dorsolateral MT dislocation.
Workup and Diagnosis
The diagnosis of high-energy Lisfranc injuries is straightforward; physical exam will reveal swelling and many times obvious deformity, including widening or flattening of the forefoot. Additionally, it might be an open injury with disruption of the skin and subcutaneous tissue. TMT joint injury and intercuneiform disruption is suggested in the presence of a gap between the first and second toes, known as a positive gap sign. Although associated vascular injury is rare, it may be difficult to palpate a dorsalis pedis pulse secondary to swelling. The clinician must also consider a concurrent compartment syndrome with severe swelling and pain with passive dorsiflexion of the toes. If unsure, measurement of pressures is warranted.
In the setting of a low-energy injury, physical exam may only reveal a patient with an inability to bear weight and possibly midfoot and forefoot swelling. Paying attention to the reported mechanism and the clinical appearance of the foot is pivotal to making the correct diagnosis. An additional finding may be plantar arch ecchymosis, which is considered pathognomonic for Lisfranc injury. To increase the accuracy of diagnosis, various tests and stress maneuvers have been described to aid in the diagnosis of subtle injury. Of note, pain on passive abduction and pronation of the forefoot is suggestive of injury to the TMT complex.
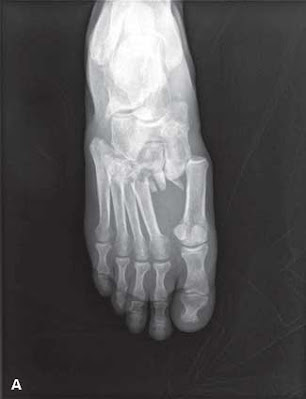
Initial imaging to obtain include nonweightbearing anteroposterior (AP), lateral, and 30-degree oblique views of the foot ( Figures 36–1A , 36–1B , and 36–1C ).
However, 50% of subtle Lisfranc injuries will have normal nonweightbearing imaging. Thus to diagnose these injuries, a weightbearing film with both feet on a single cassette or an abduction-pronation stress view should be obtained. Admittedly, these are rarely obtained secondary to pain, necessitating a bone scan or magnetic resonance imaging. Computed tomography may be beneficial as a diagnostic adjunct, as it is effective at delineating fractures.
On the AP radiograph, findings suggestive of a Lisfranc injury include incongruity at the first and second MT joints, misalignment of the medial border of the second MT and medial border of the middle cuneiform, and a diastasis of ê 2 mm between the first and second MTs as compared with the contralateral foot ( Figure 36–1A ). The oblique radiograph should show alignment of the medial border of the fourth MT and the medial border of the cuboid in a normal foot ( Figure 36–1C ). Misalignment may suggest a TMT joint complex injury. Potentially seen on this view as well as the AP is the “fleck” sign, as described by Myerson et al. It refers to the presence of a small bony fragment between the base of the second MT and the medial cuneiform and represents an avulsion of either the proximal or distal attachment of the Lisfranc ligament. The lateral radiograph will show flattening of the longitudinal arch and/or dorsal displacement at the second TMT joint ( Figure 36–1B ). The fifth MT is normally plantar in relation to the medial cuneiform. Flattening of the midfoot arch positions the medial cuneiform plantar to the fifth MT.
TREATMENT
Indications for both operative and nonoperative treatment exist, all with the goal of reestablishing a painless and stable foot. Any disruption of normal anatomy warrants surgical correction. Nonoperative treatment is limited to stable TMT joint complex injuries and include those that are nondisplaced, without fracture, and stable under radiographic stress examination. Treatment involves protected weightbearing in a Cam Walker® boot, with frequent follow-up radiographs to ensure no change in alignment. It takes approximately 4 months to recover from a nonsurgical Lisfranc injury.
In unstable Lisfranc injuries, open-reduction internal fixation is performed to restore anatomic alignment. Commonly, screw fixation is used to fix the first, second, and third TMT joints, whereas the fourth and fifth may be pinned with K-wires. Although this is one common approach to operative management, many forms of fixation are available and depend on both the nature of the injury and the surgeon’s preference. Although controversial, TMT joint arthrodesis is recommended by some for purely ligamentous Lisfranc injuries. Traditionally, this procedure was considered a salvage operation for failed ORIF and in cases of posttraumatic arthritis. Postoperatively, protected weightbearing for 3 to 5 months and therapy emphasizing passive midfoot range of motion are allowed. Regardless of the modality, anatomic alignment is the standard to decrease the risk of posttraumatic arthritis, chronic instability, and pain.
COMPREHENSION QUESTIONS
36.1 A 40-year-old equestrian complains of right midfoot pain associated with difficulty ambulating for the last 2 days, when her foot got caught in a stirrup while riding. Radiographs show a 4-mm diastasis between the first and second metatarsals. What is the most appropriate treatment?
A. Open-reduction internal fixation
B. Nonweightbearing in a short leg cast
C. Weightbearing as tolerated in an aircast
36.2 A football player who is lying on the ground after being tackled attempts to stand up. While he is still prone on the ground, another player falls directly on his left heel. He immediately experiences midfoot pain and is unable to place any weight on his left foot. In this setting, what should the team physician be most concerned about?
B. Achilles tendon rupture
36.3 A 54-year-old woman sustains a twisting injury to her foot. An AP radiograph of the foot reveals a 4-mm diastasis between the first and second metatarsals. Which structure connects the medial cuneiform to the base of the second metatarsal?
ANSWERS
36.1 A. The patient has sustained an injury to her TMT joint complex. The Lisfranc ligament, which connects the base of the second metatarsal to the medial cuneiform, has been disrupted. Anatomic reduction of the Lisfranc joint is necessary and in this case requires open reduction and internal fixation. Postoperatively, protected weightbearing for 3 to 5 months and therapy emphasizing passive midfoot range of motion are allowed. Posttraumatic arthritis, midfoot instability, and pain are the long-term outcomes of a nonreduced joint.
36.2 C. Lisfranc injuries are common in football players, with up to approximately 4% of American football players sustaining them each season. External rotation on a pronated forefoot is responsible for this and can lead to an unstable Lisfranc ligamentous injury. Other sports in which TMT joint complex injuries are encountered include equestrian events and windsurfing, in which the use of a stirrup can lead to one’s forefoot being abducted around a fixed hindfoot. When this occurs, dislocation of the second metatarsal and lateral displacement of the other metatarsals occurs.
36.3 C. This woman sustained a TMT joint complex injury, as evidenced by the large diastasis between the first and second metatarsals. The most significant and strongest ligamentous structure of the TMT joint complex is the oblique interosseous ligament, more commonly referred to as the Lisfranc ligament. Originating on the lateral surface of the medial cuneiform, it passes in front of the intercuneiform ligament and ultimately inserts on the medial aspect of the second MT base near the plantar surface. A, B, and D are incorrect—the Chopart, or bifurcate, ligament provides stability to the calcaneocuboid joint; the Deltoid ligament stabilizes the medial side of the ankle; and the Spring ligament stabilizes the talonavicular joint.
CLINICAL PEARLS
► The Lisfranc joint refers to the TMT joint complex, an osseous and capsuloligamentous network that includes the 5 metatarsals, their articulations with the cuneiforms and cuboid, and the Lisfranc ligament.
► Radiographic findings indicative of a Lisfranc injury include diastasis of ≥ 2 mm between the first and second MTs as compared with the contralateral foot, the fleck sign, flattening of the longitudinal arch of the foot, and dorsal displacement at the second TMT joint.
► The goal of both operative and nonoperative management of Lisfranc injuries is restoration of the normal anatomy of the TMT joint complex.
► Open-reduction internal fixation is the predominant surgical intervention for unstable Lisfranc injuries.
► Posttraumatic arthritis, chronic instability, and pain are the long-term complications associated with inadequate and nonanatomic reduction of the Lisfranc joint and its structures.
|
REFERENCES
Davies MS, Saxby TS. Intercuneiform instability and the “gap” sign. Foot Ankle Int. 1999;20:606-609.
Myerson MS, Fisher RT, Burgess AR, Kenzora JE. Fracture dislocations of the tarsometatarsal joints: end
results correlated with pathology and treatment. Foot Ankle. 1986;5:225-242.
Nunley JA, Vertullo CJ. Classification, investigation, and management of midfoot sprains: Lisfranc injuries
in the athlete. Am J Sports Med. 2002;30:871-878.
Ross G, Cronin R, Hauzenblas J, Juliano P. Plantar ecchymosis sign: a clinical aid to diagnose occult
Lisfranc tarsometatarsal injuries. J Orthop Trauma. 1996;10:119-122.
Thompson MC, Mormino MA. Injury to the tarsometatarsal joint complex. J Am Acad Orthop Surg.
2003;11:260-267.
Watson TS, Shurnas PS, Denker J. Treatment of Lisfranc joint injury: current concepts. J Am Acad
Orthop Surg. 2010;18:718-728.



0 comments:
Post a Comment
Note: Only a member of this blog may post a comment.