Chronic Cough/Asthma Case File
Eugene C. Toy, MD, Gabriel M. Aisenberg, MD
Case 16
A 37-year-old man presents to your office with a complaint of cough. The cough began approximately 3 months prior to this appointment, and it has become progressively more annoying to the patient. The cough is nonproductive and worse at night and after exercise. The patient has had a sedentary lifestyle but recently started an exercise program, including jogging, and he says he is having a much harder time with exertion. He “runs out of breath” earlier than he did previously and “coughs a lot”. He has not had any fever, blood-tinged sputum, or weight loss. He denies nasal congestion and headaches. He does not smoke and has no significant medical history. His examination is notable for a blood pressure of 134/78 mm Hg and lung findings of occasional expiratory wheezes on forced expiration. A chest radiograph is read as normal.
▶ What is the most likely diagnosis?
▶ How would you confirm the diagnosis?
ANSWERS TO CASE 16:
Chronic Cough/Asthma
Summary: A 37-year-old man presents to the office with
- A 3-month nonproductive cough that worsens at night and with exercise
- No fevers or other symptoms to suggest infection
- Occasional expiratory wheezes on forced expiration
- A normal chest radiograph
- No history of smoking
Most likely diagnosis: Bronchial asthma.
Confirmation of diagnosis: Spirometry with testing for bronchodilator responsiveness and bronchoprovocation testing if indicated.
- Discuss the differential diagnosis of chronic cough in adult patients. (EPA 2)
- Understand the stepwise approach to finding the cause of cough in these patients. (EPA 1, 3)
- Recognize how to diagnose and treat asthma. (EPA 3, 4)
Considerations
This is a 37-year-old man who presents with a chronic cough of more than 8 weeks’ duration. With the history of exercise intolerance, worsening cough at night, and occasional wheezes on examination, asthma is the most likely diagnosis in this patient. A chest radiograph is important to evaluate for other processes such as tumor, infection, or other etiologies of lung injury. A focused history should look for exposure to environmental irritants, medications such as angiotensin-converting enzyme (ACE) inhibitors, or other etiologies such as postnasal drip or gastroesophageal reflux disease (GERD).
APPROACH TO:
Chronic Cough
DEFINITIONS
ACUTE COUGH: Cough lasting less than 3 weeks, most commonly caused by acute upper respiratory infection but may also be caused by heart failure, pneumonia, allergic rhinitis, or exacerbation of existing structural lung disease.
ASTHMA: Condition of bronchial hyperactivity and smooth muscle hypertrophy leading to a chronic inflammatory condition of the airways associated with wide spread bronchospasm that has characteristically reversible obstruction on pulmonary function tests.
CHRONIC COUGH: Cough that often lasts more than 8 weeks. In a smoker, chronic cough is usually a symptom of chronic obstructive pulmonary disease, but bronchogenic carcinoma would be in the differential diagnosis in this population. In a nonsmoker with a normal chest radiograph and absence of ACE inhibitor use, it may be due to upper airway cough syndrome (UACS), which is usually due to postnasal drip syndrome (PNDS), GERD, or asthma.
SUBACUTE COUGH: Cough that is typically defined as lasting 3 to 8 weeks in duration and is most often infectious or postinfectious in etiology. Infectious etiologies of subacute cough include bacteria and viruses, such as respiratory syncytial virus, influenza, and adenovirus. Bacterial infections causing subacute cough are usually due to pertussis, Chlamydia, or mycoplasma.
CLINICAL APPROACH
Pathophysiology
Chronic cough is a common complaint and accounts for a large portion of health care expenditures. Physiologically, cough is a reflexive defense mechanism to clear the upper airways. The action of a cough serves two main functions: (1) to protect the lungs against aspiration and (2) to clear secretions or other material into more proximal airways to be expectorated from the tracheobronchial tree. Evaluation begins with a detailed history and physical examination, including smoking habits, complete medication list, environmental and occupational exposures, and any history of lung disease. Specific questions regarding the precipitating factors and duration and nature of the cough should be elicited. Although the physical examination or nature of the cough rarely identifies the cause, meticulous review of the ears, nose, throat, and lungs may suggest a particular diagnosis. For example, a cobblestone appearance of the oropharynx (representing lymphoid hyperplasia) or boggy erythematous nasal mucosa can be consistent with UACS. End-expiratory wheezing suggests active bronchospasm, whereas localized wheezing may be consistent with a foreign body or a bronchogenic tumor.
In more than 90% of cases, a normal chest radiograph in an immunocompetent nonsmoker guides the clinician to one of three diagnoses: UACS, asthma, or GERD. Chronic cough in an immunocompromised patient is beyond the scope of this discussion. In the outpatient setting, the mainstay of diagnosis relates to the response with empiric therapy, and multiple etiologies (UACS and GERD) are often simultaneously addressed. Often, a definitive diagnosis for chronic cough depends on observing a successful response to therapy. A rational approach includes discontinuing an ACE inhibitor if the patient is using one, obtaining a chest radiograph, and avoiding environmental irritants. If persistent, then UACS, asthma, and GERD should be considered. Referral to a pulmonologist is recommended when the diagnostic and empiric therapy options are exhausted. If suspicion for carcinoma is high, a high-resolution computed tomography (CT) scan of the thorax or bronchoscopy should be pursued. A diagnosis of psychogenic cough should be one of exclusion. See Figure 16–1 for an example of an algorithm.
Upper Airway Cough Syndrome
Upper airway cough syndrome can be attributed to sinusitis and the following types of rhinitis, alone or in combination: nonallergic, allergic, postinfectious, vasomotor, drug induced, and environmental irritant induced. Since the symptoms may be nonspecific (eg, frequent throat clearing, nasal discharge, or sensation of liquid in the throat), no definitive diagnostic criteria exist for UACS, and response to therapy confirms the diagnosis. Initial treatment for a nonallergic etiology usually includes combination treatment with a first-generation antihistamine and a decongestant for 3 weeks. For allergic rhinitis, a newer-generation antihistamine, along with a nasal corticosteroid, should be used. If the patient’s symptoms do not improve, sinus radiographs may be ordered. Opacification, air-fluid levels, or mucosal thickening could suggest sinusitis, which can be treated with antibiotics when indicated.
Asthma
Asthma is a chronic inflammatory disease of the airways characterized by air way obstruction, bronchial hyperresponsiveness, and mucus hypersecretion with recurring symptoms. These symptoms are often reversible spontaneously or with treatment.
Although wheezing is considered a classic sign of asthma, cough is often the only symptom. Cough-variant asthma usually presents with a dry cough that occurs throughout the day and night, and is worsened by airway inflammation from viral infections of the upper respiratory tract, allergies, cold air, or exercise. Although the history may be suggestive of asthma, the diagnosis should be confirmed with pulmonary function tests. Spirometry can confirm airflow obstruction with reduced forced expiratory volume in 1 second (FEV1) and FEV1/forced vital capacity (FVC); spirometry will also demonstrate reversibility with improved FEV1 after inhalation of a bronchodilator, typically a beta-agonist. Positive bronchodilator responsiveness is defined as reversible obstruction with an increase in FEV1 or FVC of more than 12% and an increase of 200 mL of volume after bronchodilator treatment. If the diagnosis is in doubt, bronchial hyperresponsiveness (the fundamental pathophysiologic abnormality in asthma) can be confirmed by a reduction in FEV1 after

Figure 16–1. Algorithm for diagnosis and treatment of chronic cough. ACEI, angiotensin-converting enzyme inhibitor; BaE, barium esophagography; GERD, gastroesophageal reflux disease; HRCT, high-resolution computed tomography; Hx, history; PE, pulmonary embolism; PNDS, postnasal drip syndrome. (Data from Irwin RS, Boulet L-P, Cloutier MM, et al. Managing cough as a defense mechanism and as a symptom: a consensus panel report of the American College of Chest Physicians. Chest. 1998;114[Suppl]:133S-181S.)
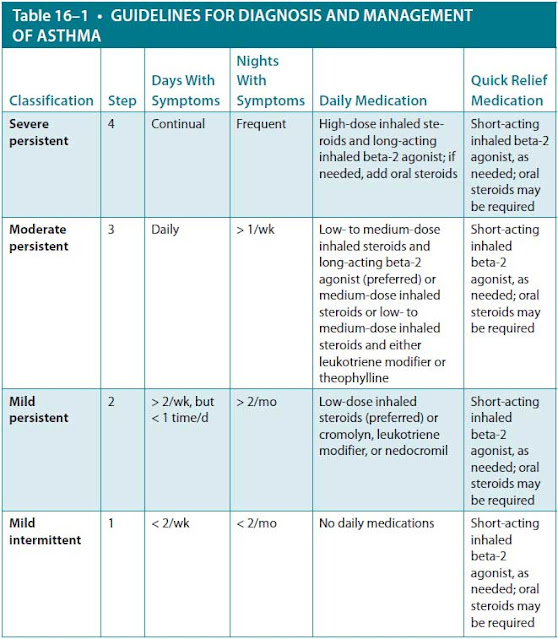
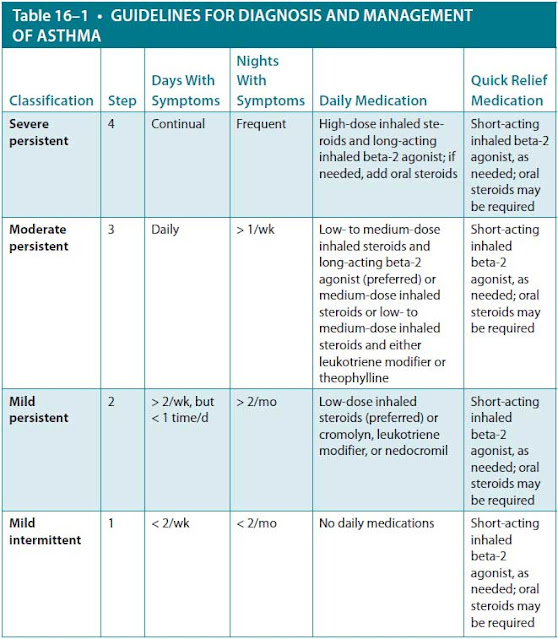
challenge with a provocative agent such as methacholine or histamine. If methacholine is used, a positive test is defined as a 20% fall in FEV1. Approach to asthma management is stepwise with use of asthma controllers such as inhaled corticosteroids (and if needed systemic corticosteroids), which inhibit airway inflammation, and bronchodilators for rapid relief of symptoms. Current guidelines emphasize a preventive approach and a stepwise approach to therapy based on asthma severity and control (Table 16–1).
Gastroesophageal Reflux Disease
Gastroesophageal reflux disease often can be clinically inapparent. It may be the primary or coexisting cause of the cough, such as the result of aspiration and vagal stimulation. Initial treatment includes lifestyle modification along with medical therapy. Recommendations include a low-fat diet, elevation of the head of the bed, avoidance of offending foods (caffeine, alcohol, chocolate), smoking cessation, and weight reduction. If the cough does not resolve with lifestyle changes, daily treatment should be initiated with an H2 receptor antagonist, such as famotidine, or a proton pump inhibitor, such as omeprazole. If acid suppression does not resolve the symptoms and if there are other symptoms of dyspepsia, a gastric motility stimulant such as metoclopramide may be considered.
Patients who remain symptomatic after maximal medical treatment may benefit from 24-hour esophageal pH monitoring to confirm the diagnosis. An esophagogastroduodenoscopy showing esophagitis or an upper gastrointestinal radiographic series demonstrating reflux further supports the diagnosis. Of note, gastrointestinal symptoms may resolve prior to resolution of the cough, and full resolution may require 2 to 3 months of intensive medical therapy.
CASE CORRELATION
- See also Case 14 (Pulmonary Embolism), Case 15 (Chronic Obstructive Pulmonary Disease), Case 17 (Pleural Effusion, Parapneumonic), and Case 19 (Community-Acquired Pneumonia).
COMPREHENSION QUESTIONS
16.1 A 21-year-old man with known asthma has been placed on a regimen consisting of inhaled corticosteroids and intermittent (short-acting) beta-2-agonist. He is being seen in the office with a new complaint of nocturnal awakenings secondary to cough and occasional wheezing. These episodes occur three to four times per week. Six months ago, his pulmonary function testing revealed an FEV1 of 80% of predicted, and FEV1/FVC of 70% of predicted. Which of the following is the best next step?
A. Oral steroids
B. Leukotriene inhibitors
C. Long-acting beta-2-agonists (LABAs)
D. Theophylline
E. Antireflux therapy
16.2 Which of the following is most accurate?
A. Cough caused by captopril may resolve with switching to enalapril.
B. Initial treatment of a chronic cough should include codeine or a similar opiate derivative to suppress the cough.
C. Cough caused by reflux can be effectively ruled out by a negative history of heartburn or dyspepsia.
D. More than one condition is often responsible for causing chronic cough in a given patient.
16.3 A 22-year-old woman presents with fatigue, arthralgias, and a nagging dry cough for the past 6 weeks, but no shortness of breath. On physical examination, her lungs are clear to auscultation, and she has bilateral pretibial tender erythematous raised nodules. Which of the following is your best next step?
A. Chest radiograph
B. High-resolution CT
C. Empiric treatment for postnasal drip
D. Antinuclear antibody test
E. Initiation of antituberculosis therapy
16.4 An obese 50-year-old man with a history of asthma is being seen in the clinic with complaints of occasional dyspepsia and nocturnal cough. He notes that he wakes up in the morning with a sour taste in his mouth. His current medications include an inhaled corticosteroid and a short-acting beta-2-agonist. Which of the following should be your next step?
A. 24-hour esophageal pH monitoring
B. Chest radiograph
C. Initiation of omeprazole
D. Short course of oral corticosteroids
E. Initiation of allergy desensitization
ANSWERS
16.1 C. Long-acting beta-2-agonists are indicated in this situation. The asthma would be classified as moderate persistent because of the exacerbations more than once a week and nocturnal symptoms more than once a week; the recommended treatment is addition of LABAs (such as salmeterol) to the inhaled corticosteroids. LABA therapy is particularly helpful with nocturnal symptoms. The logical augmentation therapy following guidelines makes the other options (answer A, oral steroids; answer B, leukotriene inhibitors; and answer D, theophylline) less useful (see Table 16–1). This patient does not show signs of GERD, so answer E (antireflux therapy) is not the best choice.
16.2 D. Often, more than one condition is responsible for causing chronic cough in a given patient. Cough from ACE inhibitors (answer A) is class dependent, and change to another class of antihypertensives is more appropriate. The etiology of chronic cough should be determined prior to suppression of the cough (answer B) because treatment of the underlying condition is the most effective approach. A patient with GERD (answer C) may present with the sole manifestation of cough, sometimes with no perceivable acid reflux.
16.3 A. The patient has clinical features suggestive of sarcoidosis given the new cough, arthralgias, and description of erythema nodosum. The initial, most cost-effective study is a chest radiograph. Hilar lymphadenopathy with or without interstitial infiltrates would solidify a diagnosis of sarcoidosis. A high-resolution CT (answer B) may be ordered if the patient has interstitial lung disease, but it is not the first study of choice. Treating postnasal drip (answer C) does not investigate the patient’s other symptoms. An antinuclear antibody test (answer D) would not necessarily identify the cause of the cough or provide a diagnosis. Antituberculosis therapy (answer E) is indicated in a patient with suspected tuberculosis. The clinical presentation of tuberculosis includes fever, night sweats, productive or bloody cough, weight loss, and exposure to a patient with tuberculosis.
16.4 C. The dyspepsia and the sour taste suggest GERD. Omeprazole is an oral proton pump inhibitor, which is a noncompetitive inhibitor of the H+-K+-ATPase (adenosine triphosphatase) pump in parietal cells and is useful in patients with GERD. Aside from acid suppression, other recommendations include dietary modifications and weight reduction. Esophageal pH monitoring for 24 hours (answer A) is indicated only if there is no response to treatment, and it is not indicated initially. Chest radiography (answer B) is only indicated if there are symptoms of cough or aspiration such as pneumonia. Answer D (short course of oral corticosteroids) is indicated with an acute exacerbation that does not respond to nebulized beta-adrenergic agonist therapy. Answer E (allergy desensitization) is indicated with patients with moderate-to-severe asthma when there is evidence of allergic reaction to various antigens.
CLINICAL PEARLS
▶ A normal chest radiograph excludes most, but not all, of the serious and uncommon causes of chronic cough.
▶ The three most common causes of chronic cough in immunocompetent nonsmokers who are not taking ACE inhibitors are UACS, asthma, and GERD.
▶ Cough caused by ACE inhibitors can be triggered after the first dose or may occur after months of therapy.
▶ Treatment of asthma is a stepwise process based on frequency of symptoms and response to prescribed medications.
▶ Asthma can be the cause of cough in a patient with a normal examination and pulmonary function tests. If suspicion is high, a positive methacholine challenge has a high predictive value.
▶ Definitive diagnosis of the etiology of chronic cough is not always necessary for successful treatment.
REFERENCES
Barnes PJ. Asthma. In: Longo DL, Fauci AS, Kasper DL, et al, eds. Harrison’s Principles of Internal Medicine. 20th ed. New York, NY: McGraw Hill; 2018:2102-2115.
Irwin RS, Bauman MH, Bolser DC, et al. Diagnosis and management of cough executive summary: ACCP evidence-based clinical practice guidelines. Chest. 2006;129(suppl 1):S1-S23.
Irwin RS, Madison JM. The diagnosis and treatment of cough. N Engl J Med. 2000;343:1715-1721.
Morice AH, Kastelik JA. Chronic cough in adults. Thorax. 2003;58:901-907.
National Heart, Lung and Blood Institute, National Asthma Education and Prevention Program. Guidelines for the Diagnosis and Management of Asthma, August 2007. https://www.nhlbi.nih.gov/health-topics/guidelines-for-diagnosis-management-of-asthma. Accessed January 15, 2020.
Williams SG, Schmidt DK, Redd SC, et al. National Asthma Education and Prevention Program. Key clinical activities for quality asthma care. Recommendations of the National Asthma Education and Prevention Program. MMWR Recomm Rep. 2003;52(RR-6):1-8.


0 comments:
Post a Comment
Note: Only a member of this blog may post a comment.