Septic Knee Case File
Eugene C. Toy, MD, Andrew J. Rosenbaum, MD, Timothy T. Roberts, MD, Joshua S. Dines, MD
CASE 19
A 56-year-old obese man presents to the emergency department for a 2-day history of progressive pain, swelling, and inability to bear weight on his right knee. The patient denies a history of recent trauma, prior knee surgery, sick contacts, or similar symptoms in the past. The patient states he has had fevers and chills over this time. His past medical history is notable for poorly controlled non– insulin-dependent diabetes and alcohol abuse. He is febrile with a temperature of 102.7°F and has an elevated heart rate of 110 beats/minute. His blood pressure is 160/95 mmHg, respiratory rate is 16 breaths/min, and oxygen saturation is 100% on room air. Examination of the knee demonstrates a swollen, erythematous, and diffusely tender right knee that is warm to palpation with painful and limited passive range of motion. Radiographs of the knee are negative for an acute fracture or dislocation but do show an effusion. The patient’s laboratory values include a white blood cell (WBC) count of 19,100 cells/μL, erythrocyte sedimentation rate (ESR) of 48 mm/hr, and C-reactive protein (CRP) of 20 mg/L. Blood cultures are pending.
► What is the most likely diagnosis?
► What is your next diagnostic step?
► What is the most appropriate initial treatment for this patient?
ANSWER TO CASE 19:
Septic Knee
Summary: A 56-year-old man with medical history significant for obesity, diabetes, and alcohol abuse presents to the emergency department febrile and tachycardic with a 2-day history of right knee pain, swelling, and an inability to bear weight. He denies any trauma or previous right knee surgery. Radiographs show an effusion but no fracture or dislocation of his right knee. Additionally, his WBC, ESR, and CRP are all elevated. Blood cultures are pending.
- Most likely diagnosis: Septic arthritis. However, the differential diagnosis also includes crystalline arthropathies (ie, gout, pseudogout) inflammatory arthridites (ie, rheumatoid, psoriatic, and reactive arthritis), tumor, occult fracture, Lyme disease, and osteoarthritis.
- Next diagnostic step: Obtaining joint fluid aspirate for analysis, including a cell count with differential, Gram stain, glucose level, and crystal analysis.
- Initial treatment: Intravenous antibiotic therapy (after obtaining blood cultures and joint fluid aspirate) and operative irrigation and drainage.
ANALYSIS
Objectives
- Be familiar with the multitude of diseases and conditions that can present similar to a septic joint.
- Understand the appropriate workup for septic joint.
- Know the treatment for a septic joint.
Considerations
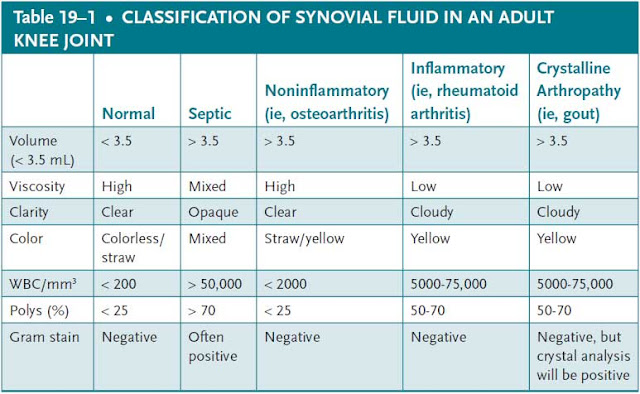
This 56-year-old male developed a grossly swollen, erythematous, and painful right knee with an inability to bear weight over the prior 48 hours. He is also febrile to 102.7°F and tachycardic. His laboratory values are abnormal and are representative of an acute infectious or inflammatory process. Furthermore, the patient’s history of poorly controlled diabetes makes him vulnerable to systemic infection. The suspicion for a septic right knee in this patient must be high. Given the history of alcohol abuse, gout is a possibility. However, his fevers and chills again favor an infectious cause of his knee pain and swelling. The patient has no history of inflammatory arthridities, such as rheumatoid arthritis, and this diagnosis is unlikely. A diagnosis of Lyme disease should always be considered in the differential for septic arthritis, but is more likely in the setting of a positive tick exposure history where the disease is endemic. Synovial fluid aspirate from this patient’s right knee will likely be consistent with septic arthritis ( Table 19–1 ), at which time intravenous antibiotics must be started and operative irrigation and drainage performed.
APPROACH TO:
Septic Knee
DEFINITIONS
SEPTIC ARTHRITIS: An orthopaedic surgical emergency most commonly caused by bacterial seeding of a joint.
OSTEOMYELITIS: An infection of bone that can cause a septic arthritis or occur as a sequela of it.
ARTHROCENTESIS: Term describing the process by which synovial fluid is obtained; also referred to as joint aspiration.
CLINICAL APPROACH
Pathophysiology
Septic arthritis most commonly occurs in the knee, followed in frequency by the hip, elbow, ankle, and, least commonly, the sternoclavicular joint. It typically occurs after bacterial seeding of the joint, but can also be caused by fungi and viruses. The 3 predominant ways by which this occurs are through direct inoculation from trauma or surgery, contiguous spread from an adjacent osteomyelitis, or in the setting of bacteremia, which is more likely to arise in immunocompromised and hospitalized individuals who have recently undergone invasive procedures.
Septic arthritis causes rapid and irreversible articular hyaline cartilage destruction in the involved joint due to the release of proteolytic enzymes from the bacteria as well as host synovial cells, chondrocytes, and inflammatory cells. Cartilage damage occurs within 8 hours of bacterial inoculation of the joint. Certain bacteria produce proteolytic enzymes such as collagenase, elastase, hyaluronidase, lipase, and lipoproteinase, which lead to cartilage destruction. Bacterial virulence factors also contribute to cartilage destruction. An example is the coagulase produced by Staphylococcus aureus, the most common pathogen responsible for bacterial septic arthritis ( Table 19–2 ). It is believed that the coagulase impairs intracapsular vascular supply due to small vessel thrombosis. The subsequent increased intracapsular pressure impedes an effective host immune response.
Clinical Presentation and Workup
Most patient’s with septic arthritis present with a relatively acute onset of a hot, swollen, and tender joint with restricted and limited range of motion and weightbearing. Systemic signs, such as fevers and chills, may also be present. In patients with concurrent bacteremia, they may appear toxic.
Radiographs are useful for ruling out other acute processes that can cause joint effusions, such as fractures and dislocation. Ultrasound is useful for confirming effusions in large joints such as the hip and for guiding aspirations. Magnetic resonance imaging will also show joint effusions and can also detect adjacent osteomyelitis.
Laboratory findings consistent with a septic joint include an elevated WBC with a left shift, ESR >30 mm/hr, and a CRP >5 mg/L. Although an elevated peripheral WBC count with increased number and percentage of polymorphonuclear leukocytes is indicative of infection, the absence of an elevated WBC does not rule out infection. Both ESR and CRP are acute-phase response markers that are elevated in the presence of infection and/or inflammation. CRP rises within a few hours of infection, reaching values up to 400 mg/L within 36 to 50 hours. It normalizes within 1 week after initiation of appropriate treatment. ESR rises within 2 days of the onset of infection and continues to rise for 3 to 5 days after appropriate antibiotic treatment is instituted. It normalizes after 3 to 4 weeks. Blood cultures should also be obtained, as bacteremia can cause septic arthritis.
Joint fluid aspiration is the gold standard for diagnosing a septic joint and helps guide antibiotic treatment and determine the need for operative intervention. It should be analyzed for cell count with a differential, Gram stain, culture, glucose level, and crystal analysis ( Table 19–1 ).
TREATMENT AND OTHER CONSIDERATIONS
Only after obtaining blood cultures and a joint aspirate should broad-spectrum, empiric antibiotic therapy commence. With organism speciation and antibiotic sensitivities, more focused antibiotic treatment and duration can be determined. Depending on institutional availability, consultation with infectious disease specialists often proves invaluable in assisting with the management of these oftentimes complicated clinical cases. Because of the rapid and irreversible cartilage damage, the diagnosis of septic arthritis requires emergent operative irrigation and drainage.
A septic joint can quickly lead to bacteremia or a systemic inflammatory response syndrome (SIRS), particularly in the immunocompromised patient. Thus, beyond orthopaedic evaluation and intervention, it is essential as a practitioner to recognize the signs of systemic compromise (ie, tachycardia, tachypnea, hypotension, end organ damage) when evaluating a patient for a septic joint.
Bacterial septic arthritis has a reported mortality of approximately 10%. Patient outcome depends not only on the type of organism involved and the general health of the individual, but also on the speed and decisiveness with which the diagnosis is made.
COMPREHENSION QUESTIONS
19.1 A 70-year-old man with a history of osteoarthritis presents to the emergency department with a 2-day history of right knee pain and swelling. He has no history of similar symptoms. He denies trauma, fever, or pain in any other joints. On examination, he is afebrile. The right knee is swollen, erythematous, and painful with passive range of motion. The remainder of the examination is unremarkable. An arthrocentesis is performed, which shows purulent fluid and a leukocyte count of 90,000/μL with 90% neutrophils. No crystals are seen on polarized microscopy. Gram stain and culture are pending. What is the most likely cause of this patient’s symptoms?
A. GoutB. PseudogoutC. Rheumatoid arthritisD. Septic arthritis
19.2 A 40-year-old intravenous drug user presents to the emergency department with a 2-day history of right knee pain with associated swelling and erythema. The patient is febrile with a holosystolic murmur at the right lower sternal border. Complete blood count reveals a leukocytosis. Blood and synovial fluid cultures are sent, and broad-spectrum antibiotics are started. Synovial fluid analysis is pending. What is the most likely pathogen causing these symptoms?
A. Neisseria gonorrhoeaeB. Staphylococcus aureusC. Pseudomonas aeruginosaD. Borrelia burgdorferi
19.3 A 50-year-old woman diagnosed with rheumatoid arthritis many years ago presents to your clinic with acute on chronic left knee pain. Her knee pain has been well controlled with anti–tumor necrosis factor therapy. She denies recent trauma, fevers, or rash. She is afebrile, and examination of the knee reveals swelling and pain with passive range of motion. What is the next most appropriate step in managing this patient’s symptoms?
A. Intraarticular steroidal injectionB. Add methotrexateC. Add nonsteroidal anti-inflammatory drugs (NSAIDs)D. Arthrocentesis
ANSWERS
19.1 D. Although the patient’s clinical presentation is consistent with a septic joint, one must consider other causes of a joint effusion in the early stages of the workup. However, the arthrocentesis, which yielded gross pus, makes a septic knee the most likely of the answer choices.
19.2 B. Gram-positive bacteria remain the most common cause of septic arthritis. Staphylococcus aureus accounts for the majority of culture-positive septic arthritis, especially within certain patient subgroups such as hemodialysis patients and intravenous drug abusers. The predominance of S. aureus in septic arthritis has remained unchanged for many years.
19.3 D. The most appropriate next step would be arthrocentesis to rule out a joint infection. Patients with rheumatoid arthritis have consistently accounted for a high percentage of patients with septic arthritis. These patients may be predisposed to septic arthritis because of poor clearance of bacteria from abnormal joints or because of phagocytic defects acquired secondary to drugs or disease.
CLINICAL PEARLS
|
► There is considerable overlap in the clinical presentation of the most common etiologies of acute joint inflammation. ► A detailed history and physical exam is vital to eliciting risk factors for septic arthritis. ► Always investigate a source of infection in suspected septic arthritis, since the pathophysiology most often involves hematogenous spread to the joint. ► Do not depend on serum markers to rule out septic arthritis. ► Arthrocentesis is vital to determining the etiology of an acutely erythematous, swollen, and painful joint. ► Do not initiate empiric antibiotic treatment without first having obtained both blood and synovial fluid specimens. |
REFERENCES
Ateschrang A, Albrecht D, Schroeter S, Weise K, Dolderer J. Current concepts review: septic arthritis of the knee pathophysiology, diagnostics, and therapy. Central Eur J Med. 2011;123:191-197.
Carpenter C, Schuur J, Everett W, Pines J. Evidence-based diagnostics: adult septic arthritis. Acad Emerg Med . 2011;18:781-796.
Lieberman JR, ed. American Academy of Orthopaedic Surgeons Comprehensive Orthopaedic Review. Rosemont, IL: American Academy of Orthopaedic Surgeons; 2009.
Salter RB. Textbook of Disorders and Injuries of the Musculoskeletal System. 2nd ed. Baltimore, MD: Williams & Wilkins; 1983:178-181.


0 comments:
Post a Comment
Note: Only a member of this blog may post a comment.