Developmental Dysplasia of the Hip Case File
Eugene C. Toy, MD, Andrew J. Rosenbaum, MD, Timothy T. Roberts, MD, Joshua S. Dines, MD
CASE 18
A young couple’s 14-month-old daughter is referred to the pediatric orthopaedic clinic by their general pediatrician because of a limp they noticed when their child ambulates. The parents cannot recall an inciting event or specific day that this began and deny any recent trauma. They state that their daughter does not appear to be in pain when she walks and has had no recent illnesses or sick contacts. The child is in good health and has met all developmental milestones up to this point, including taking her first steps at 9 months and walking independently at 12 months. Of note, this is the parent’s first child. Although the pregnancy was uncomplicated, the child was ultimately delivered at full term via cesarean section as a result of a breech presentation. The parents also state that ultrasonography for “some type of hip problem” was performed at 5 weeks of age and was normal. On exam, the left leg appears shorter than the right. Additionally, a greater degree of hip abduction is noted on the right versus the left.
► What is the most likely diagnosis?
► What is the next step in workup?
► What is the appropriate treatment of this condition?
► What physical exam maneuvers are used to diagnose this condition in newborns?
ANSWER TO CASE 18:
Developmental Dysplasia of the Hip
Summary: An otherwise healthy 14-month-old girl is brought to the clinic by her parents due to a limp. On exam, the left hip has decreased abduction compared with the right, and the left leg is shorter than the right. The parents state that this is their first child and that she was born full term via cesarean section as a result of a breech presentation. She has met all developmental milestones to this point. They also recall an ultrasound for “some type of hip problem” performed at 5 weeks of age that was negative.
- Most likely diagnosis: Developmental dysplasia of the left hip (DDH).
- Next step in workup: Anteroposterior (AP) radiograph of the pelvis.
- Treatment: Closed reduction of the left hip under general anesthesia followed by spica cast placement.
- Diagnostic maneuvers in the newborn: Ortolani and Barlow maneuvers.
ANALYSIS
Objectives
- Understand the “classic” history and presentation of DDH.
- Know the diagnostic approach to DDH.
- Understand treatment and how it differs based on patient’s age.
- Appreciate the complications associated with DDH.
Considerations
This 14-month-old child has a constellation of findings concerning for left hip pathology. The differential diagnosis of a limp in this age group must be considered here and includes both infectious and noninfectious causes. The former includes conditions such as a septic hip or osteomyelitis, whereas the latter includes transient synovitis, trauma, and DDH. Per the patient’s family, the patient has had no recent illness or been exposed to any sick contacts, making infectious causes and transient synovitis unlikely. The parents also deny any recent trauma. When entertaining the diagnosis of DDH in this patient, the birth history is significant, as DDH risk factors include female sex, breech presentation, and first-born status; this patient has all of these. The parents also state that an ultrasound done when their daughter was 5 weeks old, presumably to evaluate for DDH, was negative. This should not deter the orthopaedist from a diagnosis of DDH, as diagnosis can be delayed for multiple reasons, including late development of the pathologic changes associated with it. The same can be said for negative physical exam findings for DDH during the initial newborn screening, which is performed on all infants and includes the Ortolani and Barlow tests. Because of the significant long-term complications of DDH, a complete workup must ensue, with treatment initiated as soon as possible.
APPROACH TO:
Developmental Dysplasia of the Hip
DEFINITIONS
DEVELOPMENTAL DYSPLASIA OF THE HIP: Term describing a spectrum of developmental abnormalities of the hip joint that lead to subluxation and dislocation, predisposing patients to the development of early degenerative changes.
TRENDELENBURG GAIT: An abnormal gait associated with hip abductor weakness (ie, gluteus medius). It is characterized by the dropping of the pelvis on the unaffected side of the body at the time of heelstrike on the affected side. This lasts until heelstrike on the unaffected side, at which time lateral protrusion of the affected hip occurs. This gait can be seen in children with DDH.
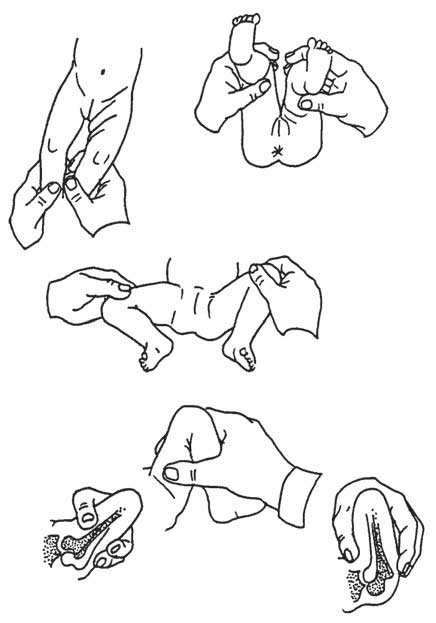
GALEAZZI TEST: Test to evaluate for DDH that is performed by flexing the infant’s knees in the supine position so that the ankles touch the buttocks ( Figure 18–1 ). If the knees are not level, the test is considered positive and indicates a possible congenital hip malformation. The test is also known as the Allis sign.
Figure 18–1. Clinical examination of developmental dislocation of the hip. In all pictures, the child’s
left hip is the abnormal side. ( A) Asymmetric skin folds; ( B) Galeazzi test; ( C) limitation of abduction; (D, E, F ) Ortolani and Barlow tests (see text). (Reproduced, with permission, from Skinner HB. Current Diagnosis & Treatment in Orthopedics . 4th ed. New York, NY: McGraw-Hill; 2006:Fig. 11-4.)
ORTOLANI AND BARLOW SIGNS: Two maneuvers used to evaluate for DDH. The Ortolani exam is a reduction maneuver that restores normal hip joint anatomy, whereas the Barlow exam is a provocative maneuver that detects an unstable hip ( Figure 18–1 ). These tests may be negative beginning at 3 months of age, despite DDH being present, due to the development of soft-tissue contractures.
CLINICAL APPROACH
Etiology
DDH is the most common orthopaedic abnormality in newborns and is the result of a disruption in the normal relationship between the acetabulum and femoral head. The incidence of DDH is reported anywhere from 1 to more than 35 per 1000 live births. DDH is most common in Native Americans and is also seen in whites. It is rare in African Americans. It is considered a multifactorial trait and is more common in females (females comprise ~80% of cases), firstborn infants, and those born in the breech presentation. The risk for DDH is increased 12-fold if a firstdegree relative has it.
The neonatal hip is unstable because of the undeveloped muscle, ligamentous laxity, and easily deformed cartilaginous surfaces comprising the joint. This relative instability, coupled with any positioning in utero that may stretch the hip capsule (as seen with the excessive flexion and adduction in a breech presentation), will predispose the neonate to subluxation or dislocation. The left hip is more frequently involved because the left femur is adducted against the mother’s lumbosacral spine when in the left occiput anterior (most common) intrauterine position. Instability results as less femoral epiphysis is contained by the acetabulum.
The femoral head displaces posteriorly and superiorly because of the pull of the gluteal and hip flexor muscles. When subluxated, this causes an asymmetric pressure that leads to a dysplastic, progressive flattening of the posterior and superior acetabular rim and medial femoral head. When dislocated, the normal, concentric motion seen at the hip joint is lost, and the joint surfaces become dysplastic with a deformed and shallow configuration.
Diagnosis
Physical exam and imaging are the mainstays of diagnosis. In the newborn, the Ortolani and Barlow tests are performed as part of the standard newborn screens. In the Ortolani maneuver ( Figure 18–1 ), the examiner will feel the dislocated hip reduce as the flexed hip is abducted while the greater trochanter is lifted anteriorly. A positive sign is a “clunk” that is often heard and felt as the femoral head reduces anteriorly into the acetabulum. In the Barlow maneuver ( Figure 18–1 ), the infant’s thigh is flexed and adducted as the examiner applies a posteriorly directed pressure. It is positive if the hip dislocates from this. Another diagnostic maneuver is the Galeazzi test, which identifies a dislocated hip via a difference in knee levels when the patient’s knees are flexed in the supine position so that the ankles touch the buttocks. This test can be used for diagnosis in older patients, unlike the Ortolani and Barlow maneuvers, which are rarely helpful after 3 months of age because of the development of soft-tissue contractures. Other physical exam findings consistent with DDH include asymmetric or limited abduction of the dysplastic hip (approximately < 70 degrees from the midline), asymmetric thigh folds and buttock creases, and leg length discrepancies in which the shorter leg is indicative of dysplasia. Once a child can walk, a Trendelenburg gait may be observed, as may a leg length discrepancy with asymmetric toe-walking on the affected side. A waddling, wide-based limp may suggest bilaterally dislocated hips.
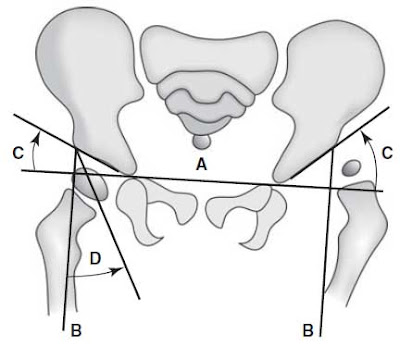
Radiography and ultrasonography are used for confirming the diagnosis. In the newborn, ultrasound is very sensitive and provides a dynamic view of the cartilaginous femoral head and acetabulum. However, it should be used only after 4 to 6 weeks of age because of the initial hip laxity associated with birth and concern for overdiagnosis. Furthermore, imaging should only be used on infants with a risk factor or physical findings concerning for DDH. Universal screening of newborns with ultrasound is not cost effective and would also lead to overdiagnosis. Plain radiographs cannot distinguish the cartilaginous components of the hip joint and should therefore only be performed when children are at least 4 to 6 months old, which is when the ossific nucleus of the femoral head can be seen on radiographs (it appears on ultrasonographic images at 12 weeks). Several lines and angles can be drawn on AP pelvic radiographs to identify DDH ( Figure 18–2 ).
Figure 18–2. Lines drawn for measurement in developmental dysplasia of the hip. In the figure, the
patient’s left hip (on the right of the figure) is the subluxated one. (A) Hilgenreiner line is a horizontal
line of the pelvis, drawn between the triradiate cartilages. The proximal femoral ossification center
should be below this line. (B ) Perkins line is a vertical line (perpendicular to Hilgenreiner line) drawn
down from the lateral edge of the acetabulum. The femoral head ossification center, as well as the
medial beak of the proximal metaphysis, should fall medial to this line. (C) The acetabular index
is the angle between Hilgenreiner line and a line joining the acetabular center (triradiate) with the
acetabular edge as it intersects Perkins line. It measures acetabular depth and should be below
30 degrees by 1 year of age and below 25 degrees by 2 years of age. (D) The center-edge angle is the
angle between Perkins line and a line joining the lateral edge of the acetabulum with the center of
the femoral head. It is a measure of lateral subluxation that becomes smaller as the hip subluxates
laterally. Normal is 20 degrees or greater. (Reproduced, with permission, from Skinner HB. Current
Diagnosis & Treatment in Orthopedics. 4th ed. New York, NY: McGraw-Hill; 2006:Fig. 11-5.)
TREATMENT
The goal of treatment for DDH is to reestablish a concentric relationship between the femoral head and acetabulum. It must begin as soon as the diagnosis is made to decrease the risk of aseptic necrosis and permanent dysplastic changes and depends on the patient’s age. From 0 to 6 months of age, treatment involves splinting the hips in flexion and abduction, which is achieved with a Pavlik harness ( Figure 18–3 ). In this position, a dislocated hip may spontaneously reduce over several weeks. The harness is used for 6 to 8 weeks or until normal hip anatomy develops. If concentric reduction is not achieved after 2 to 4 weeks, other treatment should be administered, such as closed reduction with spica casting. Closed reduction under general anesthesia with spica cast application is a treatment option for ages 6 to 18 months, as the infants are too large and strong to be controlled by a Pavlik harness. An arthrogram is used during this procedure to confirm a concentric reduction before cast application. The spica cast typically remains on for 12 weeks. If unable to obtain a concentric reduction at this time, open reduction techniques may be necessary. After 18 months of age, the femoral head and acetabulum will have developed abnormally, and open reduction is required to maintain reduction.
Figure 18–3. The Pavlik harness, a device used for treatment of hip dislocation, subluxation, and dysplasia. (Reproduced, with permission, from Skinner HB. Current Diagnosis & Treatment in Orthopedics. 4th ed. New York, NY: McGraw-Hill; 2006:Fig. 11-6.)
When DDH is untreated after 2 years of age, bony procedures involving either the acetabulum (ie, Salter, Pemberton, and Dega osteotomies), femur (ie, femoral varus derotational osteotomy), or both are required and attempt to create an environment conducive to remodeling to a more normal joint.
Complications
Ischemic necrosis is the most severe complication of DDH and can occur despite treatment. It results from compression of the vasculature supplying the capital femoral epiphysis and extreme direct pressure on the femoral head. Increased rates of ischemic necrosis are seen with forceful or excessive abduction, repeat surgery, and multiple attempts at closed reduction. Diagnosis is made based on radiographic findings, including the failure of the ossific nucleus of the femoral head to develop within 1 year after reduction, broadening of the femoral neck 1 year after reduction, and an increased density and fragmentation of an ossified femoral head.
COMPREHENSION QUESTIONS
18.1 A 15-month-old girl presents to your office for evaluation of her right hip. Which of the following is most associated with a diagnosis of developmental hip dysplasia?
A. Negative Barlow maneuverB. Asymmetry of hip abductionC. Negative Ortolani maneuverD. Increased hip abduction
18.2 Which of the following is associated with developmental dysplasia of the hip?
A. Male sexB. Vertex occiput posterior deliveryC. PolydactylyD. First born
18.3 An otherwise healthy 5-month-old infant diagnosed with developmental dysplasia of the right hip is treated in a Pavlik harness with the hips flexed to 90 degrees and abduction of 50 degrees. An AP radiograph of the pelvis at 4-week follow-up shows that the hip remains dislocated. What is your next step in management?
A. Continue treatment as is; the hip should reduce within the next 2 weeksB. Closed reduction with hip arthrogram and hip spica castingC. Open reduction with femoral shortening osteotomyD. Open reduction with pelvic acetabular osteotomy
ANSWERS
18.1 B. There are many maneuvers used to diagnose DDH, including the Ortolani and Barlow tests. However, they are rarely helpful after 3 months of age because of the development of soft-tissue contractures. Therefore, in older children one must rely on other exam findings. This includes asymmetric and limited hip abduction on the affected side.
18.2 D. Polydactyly is not associated with DDH. However, being the firstborn, female, and/or breech at birth are.
18.3 B. A 6-month-old infant who has failed treatment of DDH with a Pavlik harness after 2 to 4 weeks should be treated with closed reduction of the hip and spica casting. Continued treatment with the harness may lead to posterior acetabular erosion, a severe and devastating consequence. Both femoral and pelvic osteotomies are unnecessary in this patient and are often reserved for those 2 years of age and older with untreated DDH.
CLINICAL PEARLS
|
► DDH is considered a multifactorial trait and is more common in females (females comprise ~80% of cases), firstborn infants, and those born in the breech position. ► The risk for DDH is increased 12-fold if a first-degree relative has it. ► Diagnosis involves several exam maneuvers, including the Ortolani, Barlow, and Galeazzi tests. ► Plain radiographs cannot distinguish the cartilaginous components of the hip joint and should therefore only be performed when children are at least 4 to 6 months old, which is when the ossific nucleus of the femoral head can be seen on radiographs (it appears on ultrasonographic images at 12 weeks). ► The goal of treatment for DDH is to reestablish a concentric relationship between the femoral head and acetabulum. ► Treatment is age-dependent and includes use of a Pavlik harness when patients are < 6 months old, closed reduction and spica casting when patients are 6 to 18 months old, and open reduction when patients are > 18 months of age. After 24 months of age, reconstructive osteotomies involving the femur and/or acetabulum are often required. ► Ischemic necrosis is the most severe complication of DDH and can occur despite treatment. |
REFERENCES
Guille JT, Pizzutillo PD, MacEwen GD. Development dysplasia of the hip from birth to six months. J Am Acad Orthop Surg. 2000;8:232-242.
Vitale MG, Skaggs DL. Developmental dysplasia of the hip from six months to four years of age. J Am Acad Orthop Surg . 2001;9:401-411.


0 comments:
Post a Comment
Note: Only a member of this blog may post a comment.