Liver Cirrhosis, Probably Alcoholic Case File
Eugene C. Toy, MD, Gabriel M. Aisenberg, MD
Case 24
A 60-year-old man presents to the emergency department complaining of a 4-week history of progressive abdominal swelling and diffuse discomfort. He has no other gastrointestinal (GI) symptoms. He is a construction worker who spends at least 8 hours a day working outside. He reports that he drinks beer when he gets thirsty, usually drinking 12 cans per day. He states that he never felt the need to stop drinking alcohol. He denies illicit intravenous drug use. Over the last few months, he has noted dark colored urine, but he has not seen skin or mucosal color changes. On examination, his temperature is 100.3 °F, heart rate is 90 beats per minute, and blood pressure is 90/60 mm Hg. He is thin appearing, with telangiectasias noted on his cheeks and upper anterior chest. Yellow discoloration can be seen under his tongue and on his sclera but is not evident on his skin. His heart and lung examinations are unremarkable. The abdomen is distended, with mild diffuse tenderness, hypoactive bowel sounds, diffuse dullness to percussion, and a fluid wave. He has no peripheral or pitting edema. Laboratory studies are normal except for Na 129 mEq/L (normal 135-145); albumin 2.8 g/dL (normal 3.5-5 g/dL); total bilirubin 2 mg/dL; prothrombin time 15 seconds (normal 11-13.5); hemoglobin 11 g/dL with mean cell volume 102 fL (normal 78-95); and platelet count 78,000/mm3 (normal 150,000-500,000).
▶ What is the most likely diagnosis?
▶ What is your next step?
ANSWERS TO CASE 24B:
Liver Cirrhosis, Probably Alcoholic
Summary: A 60-year-old man presents with
- New, progressive abdominal distention
- Heavy alcohol use daily
- Scleral and mucosal icterus with physical findings consistent with ascites
- Low serum albumin and sodium
- Bilirubin slightly elevated
- Low platelet count and macrocytic anemia
Most likely diagnosis: Ascites caused by portal hypertension as a complication of hepatic cirrhosis, most likely related to alcohol abuse.
Next step: Perform a diagnostic paracentesis to evaluate the fluid to determine the likely etiology of the ascites, as well as evaluate for a known possible complication of spontaneous bacterial peritonitis (SBP).
- Explain how liver cirrhosis is diagnosed. (EPA 1, 3)
- Recognize the possible etiologies of liver cirrhosis. (EPA 2)
- Understand the utility of the serum ascites-albumin gradient (SAAG) to differentiate causes of ascites. (EPA 3)
- Outline the diagnosis of SBP. (EPA 1, 10)
Considerations
This 60-year-old man had been in good health until recently, when he noted increasing abdominal swelling and discomfort. He has drunk significant amounts of alcohol for an imprecise period of his life. Currently, he also has a low-grade fever and mild abdominal tenderness; both signs suggest a possible infection. Bacterial infection of the ascitic fluid must be considered and evaluated because untreated cases have a high mortality. Although most patients with ascites and jaundice have cirrhosis, other etiologies of the ascites must be considered, including malignancy. Diagnostic paracentesis can be used to assess for infection as well as to seek an etiology of the ascites.
APPROACH TO:
Liver Cirrhosis
DEFINITIONS
ASCITES: Abnormal accumulation (> 25 mL) of fluid within the peritoneal cavity.
CIRRHOSIS: Histologic diagnosis reflecting irreversible chronic hepatic injury, which includes extensive fibrosis and formation of regenerative nodules.
PORTAL HYPERTENSION: Increased pressure gradient (> 5 mm Hg) in the hepatic portal vein, usually resulting from resistance to portal flow and most commonly caused by cirrhosis.
SPONTANEOUS BACTERIAL PERITONITIS: Bacterial infection of ascitic fluid without any primary intra-abdominal source of infection. Occurs in 10% to 20% of cirrhotic patients with ascites.
CLINICAL APPROACH
Pathophysiology
Cirrhosis represents the end stage of chronic hepatocellular injury that results in fibrosis and architectural distortion with nodular regeneration. With ongoing hepatocyte destruction, activated hepatic stellate cells promote collagen deposition, resulting in a hardened, nodular liver that shrinks in size. Alcoholic cirrhosis is one of the most common forms of cirrhosis encountered in the United States. Quantity and duration of alcohol intake, as well as gender, genetic predispositions, and concurrent chronic hepatitis C virus (HCV) infection, contribute to the progression of alcoholic liver disease to cirrhosis. Other causes of cirrhosis are listed in Table 24–1.
When cirrhosis is suspected, patients should have an ultrasound of the right upper quadrant to assess for parenchymal changes, nodularity, hepatic cysts, and biliary ductal dilation. Histologic evaluation of tissue via percutaneous liver biopsy may be utilized for the pathologic diagnosis of cirrhosis and to differentiate the
Abbreviations: Ab, antibody; ANA, antinuclear antibody; HBeAg, hepatitis B e antigen; HBsAg, hepatitis B surface antigen; HCV, hepatitis C virus.
etiology when it is not clear by history alone. This can be helpful to diagnose hemochromatosis, Wilson disease, and autoimmune hepatitis. Increasingly, noninvasive methods of diagnosis are being utilized, including elastography to assess the stiffness of liver tissue, which correlates with hepatocellular fibrosis. Another noninvasive test utilizes blood serum biomarker measurements to assign a fibrosis score correlating with the severity of the liver fibrosis.
Clinical Presentation
Advanced liver disease will show mild elevations in AST (aspartate aminotransferase) and ALT (alanine aminotransferase), with the AST:ALT ratio greater than 2 in alcoholics, although advanced cirrhosis may eventually show normal transaminase levels due to loss of hepatocyte function. Total and direct bilirubin and alkaline phosphatase may be elevated as well. Cirrhosis will also show elevated prothrombin time, serum hypoalbuminemia, hyponatremia usually with ascites, and possibly electrolyte disturbances or impaired renal function. Patients also usually will have low platelets and macrocytic anemia.
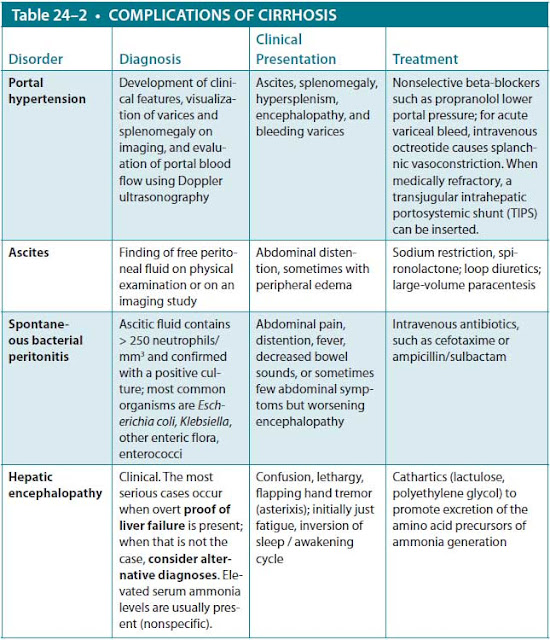
Cirrhotic patients are classified by the presence or absence of complications (Table 24–2). Compensated cirrhosis refers to patients without clinical symptoms beyond minor fatigue, muscle cramps, and itching. Decompensated cirrhosis refers to the presence of cirrhosis with complications, such as jaundice, ascites, hepatic encephalopathy, variceal bleeding, SBP, and hepatorenal syndrome. Many of these complications are driven by portal hypertension, which results from hepatocyte fibrosis causing sinusoidal resistance to portal venous flow, as well as increased splanchnic flow related to splanchnic vascular bed vasodilation.
Loss of functioning hepatic mass leads to jaundice as well as impaired synthesis of albumin (leading to edema) and clotting factors (leading to coagulopathy). Decreased liver production of steroid hormone-binding globulin leads to an increase in unbound estrogen manifested by spider angiomata, palmar erythema, and testicular atrophy and gynecomastia in men. Portal hypertension can also result in hypersplenism and splenomegaly, resulting in platelet sequestration.
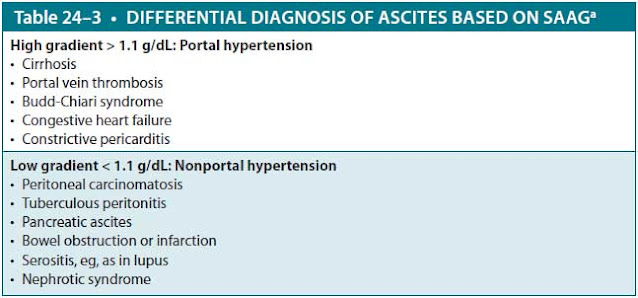
Ascites may result as a consequence of portal venous hypertension related to cirrhosis. However, it may also be a result of exudative causes, such as infection (eg, tuberculous peritonitis) or malignancy. It is important to distinguish the cause of ascites in order to look for serious and/or reversible causes, such as malignancy, and to guide therapy. Ascitic fluid is obtained by paracentesis and examined for protein, albumin, cell count with differential, and culture. The first step in trying to determine the cause of ascites is to determine whether it is caused by portal hypertension or by an exudative process by calculating the SAAG (Table 24–3).
Treatment
The treatment of ascites that is secondary to liver cirrhosis usually consists of dietary sodium restriction coupled with diuretics. Loop diuretics are often combined with spironolactone to provide effective diuresis and to maintain normal potassium levels.
Alcohol cessation is critical for those with alcoholic liver disease to prevent progression to advanced cirrhosis. Sustained abstinence after diagnosis of cirrhosis
should also be maintained to allow for possible modest reversal of fibrosis, which is occasionally seen. Ultimately, liver transplantation is the only definitive treatment for those with cirrhosis.
Patients being considered for transplant are stratified according to scoring systems to estimate disease severity and survival. The Model for End-Stage Liver Disease (MELD) score uses a patient’s laboratory values for serum bilirubin, serum creatinine, and the international normalized ratio (INR) for prothrombin time to predict survival. An older scoring system, the Child-Turcotte-Pugh system, also classifies severity of disease, with class A having the best prognosis and class C the worst.
Prevention. Men who consume > 14 alcoholic drinks per week and women who consume > 7 drinks per week should be counseled on alcohol use. A CAGE questionnaire (Cut down, Annoyed, Guilty, Eye-opener) should be utilized to assess for readiness and willingness to adopt abstinence, with referral to alcohol abstinence programs.
aSAAG, serum ascites-albumin gradient = serum albumin – ascitic albumin.
Complications
Spontaneous Bacterial Peritonitis. SBP is a relatively common complication of ascites. It is thought to be caused by translocation of gut flora into the peritoneal fluid. Symptoms include fever and abdominal pain, but often there is paucity of signs and symptoms. Diagnosis is established by paracentesis and finding more than 250 neutrophils/mm3 OR by a positive culture. Culture of ascitic fluid often fails to yield the organism (inserting fluid in a blood culture bottle raises the sensitivity from 40% to 90%). However, when positive, fluid cultures usually reveal a single organism, most often gram-negative enteric flora but occasionally enterococci or pneumococci. This is in contrast to secondary peritonitis (eg, as a consequence of intestinal perforation), which usually is polymicrobial. Empiric therapy includes coverage for gram-positive cocci and gram-negative rods, such as intravenous ampicillin/sulbactam, or a third-generation cephalosporin such as cefotaxime. Oral fluoroquinolones may also be used for uncomplicated SBP, but should be avoided in patients who were taking quinolones for SBP prophylaxis, as their organisms may be resistant. Patients who have had SBP in the past, or are considered high risk for SBP, should be maintained on a prophylactic regimen with an oral fluoroquinolone.
Esophageal and Gastric Variceal Bleeding. Other complications of advanced cirrhosis with portal hypertension include esophageal and gastric variceal bleeding, which can result in massive hemorrhage and hemodynamic instability. Treatment may include infusion of octreotide to cause splanchnic vasoconstriction and reduce portal pressure. Esophageal varices can also be treated endoscopically with ligation or banding to treat or prevent bleeding or with sclerotherapy for active bleeding. In patients presenting with upper GI variceal bleed, the incidence of SBP is higher, and these patients should be initiated on antibiotic prophylaxis. Surgical or transjugular intrahepatic portosystemic shunt (TIPS) may also be placed to decompress portal pressure and reduce the bleeding risk as the patient awaits liver transplantation.
Hepatorenal Syndrome. Hepatorenal syndrome, which typically presents as progressive decline in renal function in patients with significant ascites, can also present in advanced cirrhosis. The pathogenesis is poorly understood, though it is thought to be related to multifactorial renal vasoconstriction. Treatment is difficult, and prognosis is often poor unless patients proceed for liver transplantation.
Hepatic Encephalopathy. Hepatic encephalopathy is characterized by mental status changes, asterixis, and elevated ammonia levels related to loss of hepatic function. It may be precipitated by numerous factors, including infection such as SBP, electrolyte disturbances (hypokalemia), increased dietary protein load, and GI bleeding; it can also occur just after a TIPS procedure. Diagnosis is a clinical one based on history and physical examination and by excluding other causes of confusion. Ammonia levels are variable in patients with hepatic encephalopathy and should not be relied on to make the diagnosis. Treatment is aimed at correcting underlying causes, as well as administration of lactulose, a nonabsorbable disaccharide that causes colonic acidification and elimination of nitrogenous waste. Other cathartic agents are also effective. Poorly absorbed antibiotics such as neomycin and rifaximin are used as adjuncts in refractory cases of hepatic encephalopathy.
CASE CORRELATION
- See also Case 26 (Acute Hepatitis) and Case 27 (Painless Jaundice, Pancreatic Cancer).
COMPREHENSION QUESTIONS
24.1 A 54-year-old man with an unknown medical history is brought to the emergency department by his brother with reports that the patient has been feeling dizzy and lightheaded. His brother states that the patient has been depressed since his divorce and has been binge drinking nearly daily for the last 6 months. Last night, he came home after drinking heavily and vomited multiple times, with some blood-tinged vomit. He does not take any medications and has no known medical problems. On examination, the patient is alert but tired-appearing. Blood pressure is 94/60 mm Hg, heart rate is 126 beats per minute, respiratory rate is 16 breaths/min, and temperature is 99.3 °F. Lungs are clear to auscultation, and he is tachycardic with regular rhythm. His abdomen is distended, though soft, with quiet bowel sounds and positive shifting dullness to percussion. While being examined, the patient has a large bowel movement of black stool. Which of the following is the next best step?
A. Administer intravenous fluids.
B. Await results of hemoglobin and hematocrit.
C. Call surgery for an emergency laparotomy.
D. Give him an antiemetic for his nausea.
E. Start a proton pump inhibitor.
24.2 A 55-year-old woman with a history of decompensated alcoholic cirrhosis was admitted to the hospital 5 days ago with melena. An esophagogastroduodenoscopy (EGD) was performed, and bleeding varices were banded. The patient was started on antibiotics with ceftriaxone to prevent SBP in the setting of bleeding. Despite that fact, she developed SBP on day 3. On daily labs, her creatinine has been steadily increasing and now is at 3.1 mg/dL (1.5 on the day of admission). Despite treatment with antibiotics, holding diuretics on the day of admission, and administration of fluids and albumin, her kidney function continues to worsen. Her vital signs are normal. Physical examination shows significant ascites. Urine analysis is normal without hematuria or proteinuria. Urine Na is low (< 10 mEq/L). A renal ultrasound does not show any evidence of obstruction to urine flow. Which of the following is the definitive treatment for her condition?
A. Changing antibiotics from ceftriaxone to vancomycin and cefepime
B. Performing a TIPS procedure
C. Starting the patient on dialysis
D. Liver transplantation
24.3 A 49-year-old woman with a history of obesity and type 2 diabetes mellitus presents to the outpatient clinic with 2 to 3 months of fatigue, abdominal distention, and bilateral edema of the legs. On examination, her vital signs are normal and ascites is present, as is bilateral pitting edema of the legs. She is jaundiced and has several spider angiomas on her trunk. Her laboratory work shows mild macrocytic anemia, thrombocytopenia, and low albumin. Her liver enzymes are normal. Her liver ultrasound shows findings suggestive of fatty liver. The patient denies ever drinking alcohol. Workup of viral hepatitis is negative. What would be the best test to establish the presence of liver cirrhosis and its etiology?
A. Magnetic resonance imaging of the liver
B. Measurement of alpha-fetoprotein
C. Liver biopsy
D. CT scan of abdomen and pelvis-liver protocol
ANSWERS
24.1 A. The patient likely has an upper GI bleed from ruptured esophageal varices, related to undiagnosed alcoholic cirrhosis, based on his binge drinking history and notable ascites on examination. He is tachycardic and hypotensive, and the first step should be volume resuscitation. Awaiting laboratory results before acting would not be appropriate (answer B). He will benefit from initiation of octreotide, a somatostatin analog to decrease portal pressures, followed by early upper endoscopy. A proton pump inhibitor will not be helpful for bleeding varices (answer E). Antiemetics may improve his nausea, but it is not the most important first step (answer D). A laparotomy is not indicated for melena related to bleeding varices (answer C).
24.2 D. The patient has likely hepatorenal syndrome, and liver transplantation is the definitive treatment for this. While SBP is a known trigger for hepatorenal syndrome, antibiotics alone are unlikely to improve renal function (answer A). TIPS (answer B) will reduce portal hypertension, and dialysis (answer C) can be used to treat complications of renal failure in the setting of hepatorenal syndrome; however, neither is a definitive treatment. They can be implemented while the patient is waiting for liver transplantation.
24.3 C. The presence of diabetes mellitus and the absence of an obvious explanation for this patient’s liver dysfunction suggest liver disease resulting from fatty deposition. A liver biopsy differentiates alcoholic from nonalcoholic fatty liver, and the innocuous fatty liver from nonalcoholic steatohepatitis (which frequently progresses to cirrhosis and hepatocellular carcinoma). Despite its diagnostic value, a liver biopsy seldom alters therapeutic options. Imaging (answers A and D) and alpha-fetoprotein (answer B) have no specific etiologic diagnostic value.
CLINICAL PEARLS
▶ Alcoholic cirrhosis is one of the most common forms of cirrhosis encountered in the United States, with other notable causes including viral hepatitis and nonalcoholic fatty liver disease.
▶ Cirrhotic patients are classified by the presence or absence of complications associated with their liver dysfunction, most of which are driven by portal hypertension.
▶ An SAAG greater than 1.1 g/dL suggests the ascites is caused by portal hypertension, as seen in cirrhosis.
▶ All patients with ascites presenting to the hospital should have diagnostic paracentesis to rule out SBP, a complication of ascites and cirrhosis carrying a high mortality.
▶ SBP is characterized by the presence of greater than 250 polymorphonuclear cells/mm3 in the ascitic fluid, occasionally accompanied by positive monomicrobial culture.
▶ TIPS may be placed to decompress portal pressure to prevent esophageal variceal bleeding, but this may trigger hepatic encephalopathy.
▶ Hepatic transplant is the only cure for advanced liver cirrhosis.
▶ All patients who drink alcohol should be screened for alcohol use disorder with a CAGE questionnaire and counseled on abstinence to prevent development of alcoholic cirrhosis.
REFERENCES
Bacon BR. Cirrhosis and its complications. In: Jameson J, Fauci AS, Kasper DL, et al, eds. Harrison’s Principles of Internal Medicine. 20th ed. New York, NY: McGraw Hill; 2018: Chapter 337. http://accessmedicine.mhmedical.com/content.aspx?bookid=2129§ionid=19228381. Accessed July 7, 2019.
Dienstag JL. Chronic hepatitis. In: Kasper DL, Fauci AS, Hauser SL, et al, eds. Harrison’s Principles of Internal Medicine. 19th ed. New York, NY: McGraw Hill Education; 2015:2031-2052.
Mailliard ME, Sorrell MF. Alcoholic liver disease. In: Jameson J, Fauci AS, Kasper DL, et al, eds. Harrison’s Principles of Internal Medicine. 20th ed. New York, NY: McGraw Hill; 2018: Chapter 335. http://accessmedicine.mhmedical.com/content.aspx?bookid=2129§ionid=192283757. Accessed July 7, 2019.
Runyon BA, Umland ET, Merlin T. Inoculation of blood culture bottles with ascitic fluid improved detection of spontaneous bacterial peritonitis. Arch Int Med. 1987;147:73-75.
Tannapfel A, Dienes HP, Lohse AW. The indications for liver biopsy. Dtsch Arztebl Int. 2012;109(27-28):477-483.


0 comments:
Post a Comment
Note: Only a member of this blog may post a comment.