Posterior Hip Dislocation Case File
Eugene C. Toy, MD, Andrew J. Rosenbaum, MD, Timothy T. Roberts, MD, Joshua S. Dines, MD
CASE 3
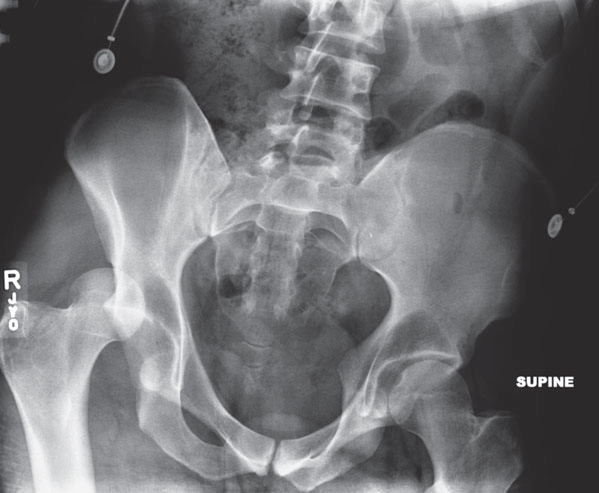
A 33-year-old male patient is brought to the emergency department (ED) by ambulance after a high-speed motor vehicle collision (MVC) that occurred approximately 2 hours ago. He was the unrestrained passenger in a car that was traveling approximately 65 miles per hour (mph) when it rear-ended a pick-up truck. There was a prolonged extrication at the scene. On arrival to the ED, the patient is writhing in pain on the gurney, complaining of right hip pain. His vital signs are within normal limits, and a trauma workup reveals deformity to the patient’s right lower extremity, but no other injuries. On examination, the patient’s right hip is slightly flexed, adducted, and internally rotated. Although he cannot extend his hip, he is able to extend his great toe, as well as dorsiflex and plantarflex his foot. His right lower extremity is warm and well perfused with brisk pulses; sensation to light touch is also grossly intact. The patient denies any prior medical or surgical history. An anteroposterior (AP) plain radiograph of the pelvis is shown (Figure 3–1).
Figure 3–1. AP radiograph of the pelvis showing a posterior dislocation of the right hip.
► What is your most likely diagnosis?
► What is the mechanism of this injury?
► What is your next step in therapy?
ANSWER TO CASE 3:
Posterior Hip Dislocation
Summary: A 33-year-old male patient is brought to the ED 2 hours after a high-speed MVC and prolonged extrication complaining of right hip pain. On exam, his right lower extremity is slightly flexed, adducted, and internally rotated. It is neurovascularly intact. An AP radiograph of his pelvis identifies a right hip dislocation.
- Most likely diagnosis: Posterior dislocation of the right hip
- Mechanism of injury: Axial load on a flexed hip (a dashboard injury)
- Next step in therapy: Emergent closed reduction within 6 hours to decrease the risk of femoral head osteonecrosis and sciatic nerve injury
ANALYSIS
Objectives
- Know the diagnostic approach to hip dislocations.
- Understand that a native hip dislocation is an orthopaedic emergency.
- Be familiar with the technique used to reduce a dislocated hip.
- Know the postreduction workup and management.
- Know the complications associated with hip dislocations.
Considerations
This 33-year-old male patient presents to the ED with a right hip dislocation 2 hours after a high-speed MVC. The first priority is a trauma workup, applying advanced trauma life support (ATLS) principles. This patient has no other injuries, and therefore, the next step must be to evaluate the imaging obtained to rule out an associated femoral neck fracture, followed by emergent reduction. It is imperative that the orthopaedist perform a complete and well-documented physical examination, noting any neurovascular compromise or other injuries to the right lower extremity before reduction. Successful reduction is dependent on the ability of ED physicians to perform conscious sedation with good muscle relaxation. If they are unable to do this, the patient may require reduction in the operating room under general anesthesia. A repeat AP pelvis radiograph should be obtained to confirm reduction, followed by a computed tomography (CT) scan through the acetabulum. This will evaluate for a concentric reduction and the presence of any intra-articular fragments and associated fractures of the femoral head and acetabulum. After reduction, the patient’s hip should be ranged and assessed for stability and a repeat neurovascular exam performed. The patient must be counseled on the risk of osteonecrosis of his hip, the high association of this injury with other injuries (ipsilateral knee injuries are common), and hip precautions.
APPROACH TO:
Hip Dislocation
DEFINITIONS
OSTEONECROSIS (AVASCULAR NECROSIS): Process by which bone tissue dies due to either a temporary or permanent disruption to the bone’s blood supply. It is associated with excessive steroid use, sickle cell disease, alcoholism, deep diving (caisson disease), Gaucher disease, lupus, and rheumatoid arthritis. It can also be posttraumatic, such as after a hip dislocation, or idiopathic in nature.
HIP PRECAUTIONS: Restrictions designed to prevent posterior dislocation of the hip. They are applied after total hip arthroplasty performed via a posterior approach as well as after native posterior hip dislocations. The precautions prohibit patients from crossing their legs, bending their hip past a 90-degree angle, and twisting their hip inward.
ALLIS MANEUVER: One of several described methods by which to reduce a dislocated hip. The patient is placed in the supine position, and the pelvis is stabilized by an assistant applying pressure. The physician then applies in-line longitudinal traction to the femur followed by gentle flexion of the hip to 90 degrees. Internal and external rotation of the hip ensues, with continued traction until reduction is achieved. Reduction is often signified by an audible and palpable clunk.
CLINICAL APPROACH
Etiology and Mechanism of Injury
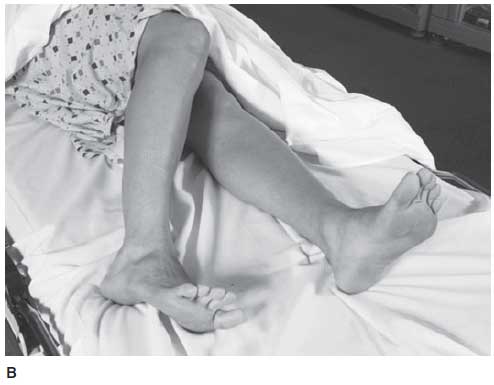
Posterior hip dislocations are caused by high-energy mechanisms and comprise greater than 90% of all native hip dislocations (Figure 3–2). They are referred to as dashboard injuries because of their high association with motor vehicle accidents in which the patient is subjected to an axial load on a flexed hip occurring when the knee is driven violently into the dashboard. Other causes include falls and athletic injuries. In all of these instances, the hip is positioned in a flexed, adducted, and internally rotated position (Figure 3–2). Anterior dislocations, which are uncommon and comprise fewer than 10% of hip dislocations, occur via an external rotation and abduction force and are not discussed.
Anatomy
The inherent stability of the hip joint is provided by its ligamentous, bony, and muscular architecture, as well as the labrum. Its main blood supply is via the medial femoral circumflex artery, with other contributions from the lateral femoral circumflex artery, artery of the ligamentum teres (obturator), and the inferior and superior gluteal arteries. The sciatic nerve lies close to the hip joint, exiting anterior to the piriformis in the greater sciatic notch.
Figure 3–2. Posterior dislocation of the hip. (A) Posterior dislocation of the hip. (B) The clinical
appearance of a posterior dislocation of the right hip. (Reproduced, with permission, from Tintinalli J,
et al. Tintinalli’s Emergency Medicine: A Comprehensive Study Guide. 7th ed. New York, NY: McGraw-Hill; 2010:Fig. 270–12.)
Initial Management, Diagnosis, and Classification
Given their high-energy mechanisms, ATLS protocol must be followed in the initial management of the patient presenting with a hip dislocation. After this, a complete physical exam is performed, and in the setting of a posterior hip dislocation, the position of the patient’s affected extremity is often telltale. The limb will be flexed, adducted, and internally rotated. Neurologic and vascular status must be documented. An AP pelvic radiograph should be obtained and will confirm the diagnosis. With posterior dislocations, the femoral head appears smaller than its contralateral side, joint congruency is lost, and the lesser trochanter difficult to visualize as a result of the internal rotation of the femur. The femoral neck of the affected side must be adequately visualized and evaluated for fracture, as this would change the treatment plan and require operative intervention.
The Thompson and Epstein classification for hip dislocation is one of the most widely used, based on radiographic characteristics, and is described in Table 3–1.
Treatment and Postreduction Management
A hip dislocation is an orthopaedic emergency, and closed reduction attempts must be performed as soon as possible to reduce the period of avascularity to the hip. It must be reiterated, however, that adequate imaging be obtained before any reduction attempts to rule out an ipsilateral femoral neck fracture. Reduction can be performed in the ED if conscious sedation and muscle relaxation can be achieved. If adequate sedation and relaxation is unattainable in the ED, the hip must be reduced in the operating room under general anesthesia.
There are many described reduction techniques for posterior dislocations, including the Allis and Bigelow maneuvers and the East Baltimore lift. In the Allis maneuver, which requires the patient to be supine on the table, the patient’s pelvis is stabilized by an assistant applying pressure. The physician then applies in-line longitudinal traction to the femur followed by gentle flexion of the hip to 90 degrees. Internal and external rotation of the hip ensues with continued traction until reduction is accomplished. Reduction is often signified by an audible and palpable clunk.
A repeat AP pelvic radiograph must be obtained to confirm a successful reduction. Once this is confirmed, the hip should be ranged gently to assess stability and a CT scan performed to evaluate for a concentric reduction, the presence of intraarticular fragments, and the presence of femoral head and acetabular fractures.
Posterior acetabular wall fractures with > 40% wall disruption lead to an unstable hip, whereas it remains stable when < 20% of the wall is disrupted. An irreducible hip dislocation, which is caused by bony or soft-tissue interposition within the joint, requires emergent open surgical intervention to reduce the pressure on the hip’s articular cartilage and subsequent risk for avascular necrosis. A nonconcentric reduction may also require open operative intervention or skeletal traction for the same reasons seen with irreducible hips.
If the hip is found to be clinically and radiographically stable after reduction, an abduction pillow or knee immobilizer must be used to prevent inadvertent movements by the patient that could compromise reduction and cause recurrent dislocation. Strict hip precautions should be enforced at all times and prohibit patients from crossing their legs, bending their hip past a 90-degree angle, and twisting their hip inward.
There is no one specific approach to rehabilitation after a hip dislocation, and the patient’s weight-bearing status and need for postreduction traction or bed rest are controversial and surgeon dependent.
Complications
The risk of developing posttraumatic osteonecrosis of the femoral head is what makes hip dislocations an orthopaedic emergency. The critical time to reduction, which in theory will restore blood flow to the femoral head, has not been definitively determined. However, it is thought that a greatly increased risk of avascular necrosis occurs with a delay in reduction of greater than 6 to 12 hours. It is important to note that those who incur hip dislocations via higher energy mechanisms are more likely to develop osteonecrosis as a result of greater initial damage to the surrounding blood supply. Osteonecrosis commonly occurs within 2 years. Other complications include development of posttraumatic arthritis, sciatic nerve palsy, and recurring dislocations. Furthermore, many patients presenting with hip dislocations have other significant systemic injuries as well as ipsilateral knee and bony injuries.
COMPREHENSION QUESTIONS
3.1 A 45-year-old driver is involved in a motor vehicle collision and sustains a posterior dislocation of the left hip. What is the most likely concomitant injury?
A. Lumbar burst fractureB. Right knee meniscus tearC. Left knee anterior cruciate ligament tearD. Subdural hematoma
3.2 A 28-year-old man is about to be discharged from the hospital after a motor vehicle collision in which he sustained a right hip dislocation. Before leaving, he asks to review what positions he can and cannot place his hip. You explain to him that posterior hip precautions prohibit:
A. Leg crossingB. Flexing the hip to greater than 90 degreesC. Twisting the hip inwardD. Hip extensionE. A, B, and C
3.3 A 41-year-old woman sustains a left posterior hip dislocation. After a successful attempt at closed reduction in the emergency room using conscious sedation, what is the next step in management?
A. CT scan of the hip and pelvisB. Hip spica cast applicationC. Further evaluation of hip stability via an exam under anesthesia in the operating roomD. Femoral skeletal traction pin
ANSWERS
3.1 C. The traumatic hip dislocation in this case is due to a dashboard injury in which the forces are first transmitted through the knee en route to the hip. Thus the possibility of a concurrent ipsilateral knee injury should be explored through careful clinical examination and possibly magnetic resonance imaging.
3.2 E. Choices A, B, and C are posterior hip precautions. Hip extension is not and can be performed by those who have had a posterior dislocation or have undergone hip replacement via a posterior approach. However, it is considered an anterior hip precaution and therefore should not be done in those who undergo hip replacement via an anterior approach or who have dislocated anteriorly.
3.3 A. The next step in management after reduction of a posterior hip dislocation is obtaining a CT scan to evaluate for damage (ie, fracture or impaction deformity) to the femoral head and acetabulum. Furthermore, a CT scan will identify an incongruent reduction and free intraarticular joint fragments. Such findings may require additional intervention.
CLINICAL PEARLS
► Posterior hip dislocations are caused by high-energy mechanisms and comprise greater than 90% of all native hip dislocations. ► In the setting of a posterior dislocation, the hip is positioned in a flexed, adducted, and internally rotated position. ► A hip dislocation is an orthopaedic emergency, and closed reduction attempts should be performed as soon as possible to reduce the period of avascularity to the hip. ► An AP pelvic radiograph must be obtained to confirm reduction, and a CT of the hip should be done to evaluate joint congruency, presence of intraarticular fragments, and presence of femoral head and acetabular fractures. ► Posterior hip precautions prohibit patients from crossing their legs, bending their hip past a 90-degree angle, and twisting their hip inward. ► Complications associated with hip dislocations include osteonecrosis, posttraumatic arthritis, sciatic nerve palsy, and recurring dislocations. |
REFERENCES
Foulk DM, Mullis BH. Hip dislocation: evaluation and management. J Am Acad Orthopaed Surg. 2010;18(4):199-209.


0 comments:
Post a Comment
Note: Only a member of this blog may post a comment.