Distal Radius (Colles) Fracture Case File
Eugene C. Toy, MD, Andrew J. Rosenbaum, MD, Timothy T. Roberts, MD, Joshua S. Dines, MD
CASE 2
A 32-year-old right-hand-dominant female was standing on a stool in her kitchen, lost balance, and fell onto her outstretched right hand. She arrives at an urgent care clinic and is complaining of pain and deformity about her wrist. She did not sustain any other injuries and has no significant past medical history. Physical exam reveals her right wrist to have intact skin, and it is swollen and ecchymotic. She has significant tenderness to palpation about the wrist, which has a mild, dorsally angulated deformity. There is no snuffbox tenderness. She readily flexes her distal interphalangeal joints and abducts her fingers. She weakly extends the thumb and fingers. There is brisk capillary refill throughout, and sensation is intact in the median, radial, and ulnar nervous distributions. Anteroposterior (AP) and lateral wrist films are obtained and can be seen in Figure 2–1.
Figure 2–1. AP and lateral plain radiographs of a right wrist in a skeletally mature individual.
► What is the most likely diagnosis?
► What additional injuries are you most concerned about?
► What is the most appropriate initial treatment for this patient?
ANSWER TO CASE 2:
Distal Radius (Colles) Fracture
Summary: A 32-year-old, right-hand-dominant female sustained a wrist injury after falling on an outstretched hand. She has pain and a dorsally angulated deformity about the distal radius. Wrist x-rays show an intraarticular distal radius fracture with concomitant ulnar styloid fracture.
- Most likely diagnosis: This is an intraarticular distal radius fracture that involves the distal radioulnar joint (DRUJ) with a concomitant ulna styloid fracture. This may be classified as a Frykman type VI distal radius fracture.
- Additional injuries to be concerned: Scaphoid fractures, radial head fractures (Essex Lopresti), elbow dislocation, proximal humerus fractures, shoulder dislocations, and clavicle fractures.
- Initial treatment: All displaced fractures should undergo closed reduction. A hematoma block with or without sedation provides analgesia for closed reduction. The goals of reduction include anatomic repositioning of fragments for healing, limiting postinjury swelling and pain, and relieving compression on median nerve and other surrounding neurovascular structures.
ANALYSIS
Objectives
- Understand the anatomy of the distal forearm and proximal wrist.
- Be familiar with basic treatment options for distal radius fractures with regard to both nonoperative and operative management.
- Recognize potential complications arising from initial injuries and their treatments.
Considerations
This 32-year-old patient sustained an injury to her dominant hand from a fall. Because the patient will be focused on her wrist, it is important to remember to evaluate the entire extremity, focusing on areas of potential injury such as the snuffbox, elbow and radial head, shoulder, and clavicle. If warranted by mechanism, full trauma workup should be initiated. A careful history should elucidate whether the patient suffered a simple mechanical fall or whether there were underlying etiologies behind her accident, such as syncope or gait instability. Examination of the skin is important to ensure that there is not an open fracture that would necessitate urgent operative debridement and washout. Next, a careful neurovascular exam needs to be performed. Extension of the thumb by the extensor pollicus longus should be evaluated because the tendon can be trapped or lacerated as it passes the Lister tubercle. Particular attention should be paid to the median nerve. Carpal tunnel compression symptoms are common secondary to forced hyperextension of the wrist, as well as local hematoma formation, impingement by fracture fragments, and increased compartment pressures.
Finally, after a complete and thorough exam is performed and documented, the fracture should be immobilized, regardless of whether it meets requirements for operative fixation. This is typically performed by cast or splint immobilization.
APPROACH TO:
Distal Radius Fracture
DEFINITIONS
COLLES FRACTURE: An eponym originally describing extraarticular fractures of the distal radius. More commonly used today as a lay term for any dorsally angulated distal radius fracture.
SMITH FRACTURE: An eponym for volarly angulated distal radius fractures, most commonly incurred after a fall or blow to the dorsum of the wrist. This is sometimes referred to as a reverse Colles fracture.
CHAUFFEUR FRACTURE: An avulsion fracture of the radial styloid, historically as the result from hand-cranked automobiles in which engine backfire forced the crank back into the chauffeur’s hand. Also known as a “backfire” or Hutchinson fracture. Today these result from falls onto outstretched hands, with axial compressive force driving the scaphoid into the radial styloid as the wrist is both ulnarly deviated and dorsiflexed.
BARTON FRACTURE: A shear fracture of the volar or dorsal lip of the distal radius, resulting in dislocation or subluxation of the wrist, most commonly in the volar direction.
CLINICAL APPROACH
Anatomy and Mechanisms of Injury
The distal radius consists of the metaphysic, or metaphyseal region, as well its articulating surfaces, which include the scaphoid facet, lunate facet, and the sigmoid notch. The metaphysics flares distally, and its cortical bone becomes thin, especially at its dorsal and radial aspects. Thin bone at this region is prone to comminution, and therefore, many distal radius fractures eventually collapse dorsoradially, despite initial anatomic reductions.
Radiographic Evaluation
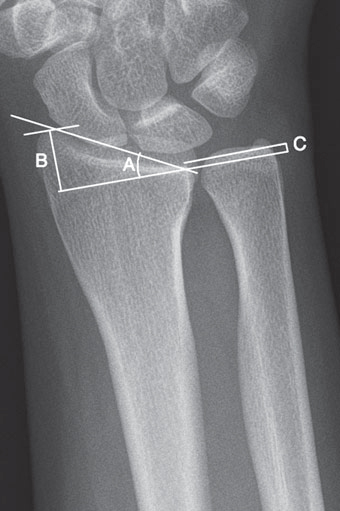
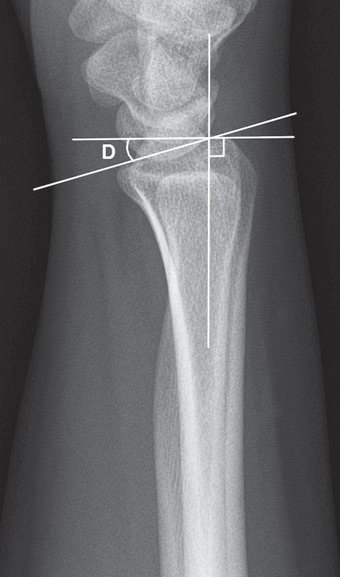
Several distal radius and ulna measurements are helpful in evaluating the severity of injury and can later be used to assess reduction. Although these values are wellestablished, they can vary greatly between individuals. If doubt exists regarding the adequacy of alignment, contralateral comparison views should be obtained. Figures 2–2 and 2–3 are AP and lateral radiographs of normal wrists, respectively, showing measurements of the following alignment parameters:
Figure 2–2. An AP plain radiograph of a normal wrist showing the radiographic measurements: radial
inclination (A), radial length (B), and ulna variance (C).
Figure 2–3. A lateral plain radiograph of a normal wrist with measurement of palmar tilt (D).
1. Radial inclination (normally 23 degrees). Measured on an AP wrist film as the angle between a line drawn from the radial styloid to the medial corner of radius and a line drawn perpendicular to long axis of radius.
2. Radial length (normally 12 mm). Measured on an AP wrist film as distance in millimeters between the tip of the radial styloid and most distal point of the ulnar head of the radius.
3. Ulnar variance (normally ± 0-2 mm). On AP: distance between medial corner of the articular surface of the radius and most distal point of articular surface of the ulnar head.
4. Dorsal/palmar tilt (normally 11 degrees). On true lateral: angle between line perpendicular to the long axis of radius and line from most distal points of volar and dorsal lips of radius. Palmar tilt is the most important parameter to restore, as it has the greatest bearing on functional outcome.
Classification
Several distal radius fracture classification schemes exist, including informal descriptive classifications to formal systems based on mechanism (Fernandez classification) or extent of articular involvement (Frykman classification). Often, fractures of the distal radius are described with regard to whether the fracture is open or closed, intraor extraarticular with regard to the radiocarpal joint and/or the DRUJ, whether the fracture is comminuted or simple, the direction of displacement if present, and whether there is an associated ulna styloid fracture.
TREATMENT
Nonoperative Treatment
Closed reduction and cast immobilization is the mainstay of treatment. All displaced distal radius fractures should have attempted closed reduction, regardless of severity. If swelling is significant or if superficial skin injury is present, fractures may be initially splinted with delayed casting. Nondisplaced fractures may be cast in situ, typically with a short arm cast. If the fracture remains stable with the acceptable radiologic parameters discussed previously, then fractures may be treated definitively with a cast. Acceptable parameters for active, healthy patients include restoration of palmar tilt, a neutral tilt or up to 10 degrees of dorsal angulation, restoration of radial length within 2 to 3 mm of the contralateral wrist, the absence of intraarticular step off > 1 to 2 mm, and less than a 5-degree loss of radial inclination.
Close follow-up with serial radiographs is necessary, as some fractures have a tendency to collapse. As mentioned, even the most anatomic of reductions may collapse in the setting of dorsal comminution and other types of metaphyseal comminution or bone loss. For low-demand, elderly patients in whom the risks of surgery outweigh the benefits, fractures may be treated definitively with a cast, splint, or brace.
Operative Treatment
Several modes of operative treatment exist, including plate fixation, percutaneous pinning, and even external fixation. The current mainstay of treatment is an open-reduction internal fixation with plate and screws that may be placed either dorsally or volarly. Surgical indications include metaphyseal instability, especially with comminuted dorsal-medial cortices; intraarticular fractures with articular step off > 1 to 2 mm or significant comminution; open fractures; DRUJ instability; or secondary loss of reduction with loss of radial inclination of > 5 degrees, loss of radial length of > 2 to 3 mm, or dorsal angulation > 10 degrees. Additional relative indications include bilateral fractures, an impaired contralateral extremity, and associated carpal fractures.
OUTCOMES AND COMPLICATIONS
Several factors are associated with elevated risk of re-displacement after closed reduction of a distal radius fracture. These include patient age > 80 years, significant displacement before initial reduction, significant metaphyseal comminution, and immediate displacement after reduction requiring multiple attempted reductions.
Malunion is a significant complication after nonoperative treatment. Malunion can lead to negative effects on radiocarpal mechanics, loss of motion, and pain at the DRUJ. Acute carpal tunnel syndrome that does not resolve soon after reduction may lead to median nerve damage.
Posttraumatic osteoarthritis is a common sequelae of all intraarticular fractures and correlates strongly with inadequate articular reduction. Anatomic restoration of the articular surface is paramount for long-term functional success.
Complex regional pain syndrome (CPRS) may develop. Cardinal features of CPRS include abnormal or neuropathic pain, temperature changes, abnormal localized diaphoresis, joint stiffness/atrophy/swelling, and bone changes. Tendon rupture and tenosynovitis can occur, most frequently involving the extensor pollicus longus (EPL) tendon. A higher risk of EPL rupture is associated with dorsal plating versus volar plating when surgical fixation is performed, because prominent dorsal plates may lead to repetitive wear on the tendon, leading to eventual rupture. EPL rupture may also occur in the absence of internal fixation, because callus formation from even minimally displaced fractures and vascular disruption may lead to gradual tendinous attrition and eventual rupture.
COMPREHENSION QUESTIONS
2.1 A 27-year-old right-hand-dominant man sustains a right distal radius fracture after a trip and fall. He is treated with closed reduction. Which radiographic parameter has the greatest bearing on functional outcome?
A. Radial heightB. Radial inclinationC. Ulnar varianceD. Palmar tiltE. Bauman angle
2.2 A 50-year-old engineer suffers a comminuted distal radius fracture that fails an initial attempt at cast immobilization. He undergoes elective open-reduction internal fixation of the fracture with a dorsal plating technique. Which tendon is most likely to rupture after dorsal plate fixation of a distal radius fracture?
A. Flexor carpi radialisB. Extensor pollicus longusC. Abductor pollicus longusD. Extensor pollicus brevisE. Extensor digitorum
2.3 A 52-year-old female fell from her bicycle while trying to light a cigarette while navigating a busy intersection. She suffers a right-sided, dominant distal radius fracture. The fracture is closed and simple, extends into the radiocarpal joint, and is almost 100% displaced dorsally. On additional radiographs, she has a small, nondisplaced fracture of her ipsilateral radial head. Which of the following, if present, is associated with the highest risk of displacement after closed reduction and cast immobilization?
A. Intraarticular involvementB. Age > 50 years oldC. The severity of prereduction dorsal displacementD. Ipsilateral fracture of the radial headE. Tobacco history
ANSWERS
2.1 D. Although radial height, radial inclination, and ulnar variance are important reduction parameters for the successful nonoperative treatment of distal radius fractures, palmar tilt has been shown to have the greatest bearing on long-term functional outcomes. Bauman angle is found in the pediatric elbow and is most commonly used to assess supracondylar fractures. Bauman angle is measured between the axis of the humeral shaft and the physis of the lateral condyle.
2.2 B. The extensor pollicus longus has been shown to be more prone to rupture with dorsal plating than the fl exor carpi radialis, abductor pollicus longus, extensor pollicus brevis, and the extensor digitorum. EPL rupture is thought to occur secondary to repetitive wear of the tendon on a prominent plate. Although several different methods are described, irreparable EPL ruptures may be treated with transfer of the redundant extensor indicis proprius to the thumb to regain thumb extension.
2.3 C. Of the several factors associated with re-displacement after closed reduction of distal radius fractures, the severity of initial displacement is likely the most significant. Additional risk factors include patient age > 80 years (not 50 years), significant metaphyseal comminution (she had a simple, 2-part fracture), and immediate displacement after reduction requiring multiple attempted reductions (not mentioned in the vignette). Intraarticular involvement, positive tobacco history, and even concomitant fractures have not been clearly associated with a high risk of failed closed reduction.
CLINICAL PEARLS
► Distal radius fractures are amongst the most common fractures treated in the United States at more than 650,000 cases per year. ► Patients with distal radius fractures may have incurred more than a simple wrist injury, especially in high-energy trauma scenarios. It is therefore essential to assess similarly injured structures such as the scaphoid, radial head, shoulder, and clavicle. ► The incidence of distal radius fractures as the result of simple falls mirrors that of hip fractures. Both may be evidence of osteopenia or osteoporosis, and patients at risk should be worked up accordingly. |
REFERENCES
Buchholz RW, Court-Brown CM, Heckman JD, Tornetta P, eds. Distal radius and ulna fractures. In: Rockwood and Green’s Fractures in Adults. 7th ed. 2 vol. Philadelphia: Lippincott Williams & Wilkins; 2010:829-880.
Egol KE, Koval KJ, Zukerman JD, eds. Distal radius. In: Handbook of Fractures. 4th ed. Philadelphia: Lippincott Williams & Wilkins; 2010:269-280.


0 comments:
Post a Comment
Note: Only a member of this blog may post a comment.