Posterior Communicating Artery Aneurysm Case File
Eugene C. Toy, MD, Ericka Simpson, MD, Pedro Mancias, MD, Erin E. Furr-Stimming, MD
CASE 32
You are paged to the emergency center (EC) to evaluate a 38-year-old woman for blurry vision. She first noticed the vision change when she woke up this morning, but it was not overly concerning for her. However, when she arrived at work, her coworker noted that her eyelid seemed to be drooping and that her pupils were not the same size. She contacted her primary care physician, who recommended that she should proceed directly to the emergency room (ER) for evaluation. She denies any other symptoms and has a past medical history significant only for migraine headaches. These headaches have not changed in character or frequency. On examination, her left eyelid is slightly lowered and the left pupil is larger than the right. The left eye is also slightly deviated laterally and downward and exhibits reduced adduction and vertical movements. She denies any eye pain. The rest of the neurologic and physical examination is normal. A computed tomography (CT) scan without contrast is normal. On further questioning, she mentioned that her mother had an aneurysm repaired years ago.
▶ What is the most likely diagnosis?
▶ What is the next diagnostic step?
ANSWERS TO CASE 32:
Posterior Communicating Artery Aneurysm
Summary: A 38-year-old woman presents with symptoms of ptosis, dilated pupil, and blurry vision. She is noted to have restricted extraocular movements on examination. These findings all localize to the third cranial nerve. CT of the head is normal.
- Most likely diagnosis: Third nerve palsy due to posterior communicating artery aneurysm.
- Next diagnostic step: Magnetic resonance imaging (MRI) and magnetic resonance angiogram (MRA) of the brain.
- Be familiar with common etiologies for anisocoria and how to differentiate them.
- Understand the physiology of pupillary reaction.
- Understand the diagnostic evaluation of third nerve palsy, including imaging studies.
Considerations
This 38-year-old woman presents with acute ptosis, dilated pupil, and restricted extraocular movements, which are all findings that localize to the third cranial nerve. Parasympathetic fibers that constrict the pupil are located on the outside surface of the nerve, and therefore pupillary involvement in a third nerve palsy suggests a compressive lesion. Any acute-onset third nerve palsy with pupillary involvement is considered a neurologic emergency due to the possibility of an aneurysm, most commonly of the posterior communicating artery. Motor fibers controlling extraocular movements run in the body of the nerve. Therefore, with a microvascular ischemic lesion to the nerve, deeper nerve fibers are affected, and pupil involvement is less common. Furthermore, if a lesion occurs in a distal branch of the third nerve, the patient may only have a “partial third nerve palsy.” Suspicion for a life-threatening etiology of third nerve palsy is low when the pupil is spared or the signs of a partial third nerve palsy clearly localize to a particular branch of the nerve.
DEFINITIONS
ANISOCORIA: Unequal pupil size.
MIOSIS: Constriction of the pupil.
MYDRAISIS: Dilation of the pupil.
ADIE PUPIL: Tonic pupil that has poor reaction to light but will accommodate on near gaze. It is slow to dilate after constriction. This is due to damage to the parasympathetic ciliary ganglion or short ciliary nerves followed by aberrant reinnervation. Idiopathic cases of tonic pupil are referred to as Adie pupil.
CLINICAL APPROACH
Physiology
The size of the pupil depends on a balance between parasympathetic and sympathetic tone. Both of these subsets of the autonomic nervous system interface with antagonistic muscles, which determine the size of the pupil. The pupillary sphincter muscle is innervated by the parasympathetic nervous system, and its activation results in pupillary constriction or miosis. The dilator muscle, on the other hand, is innervated by the sympathetic nervous system, and its activation results in pupillary dilation, otherwise known as mydriasis.
The cell bodies for the parasympathetic preganglionic neurons are located in the Edinger-Westphal nucleus of the upper midbrain. These axons join the ipsilateral oculomotor nucleus motor fibers to form the third cranial nerve. Throughout the course of the oculomotor nerve, the parasympathetic fibers are situated superficially (immediately internal to the epineurium) and are susceptible to compressive injury. These parasympathetic axons eventually synapse in the ciliary ganglion, which houses the cell bodies of the postganglionic neurons. Postganglionic nerve axons then emerge to form the short ciliary nerves, which innervate the sphincter muscle.
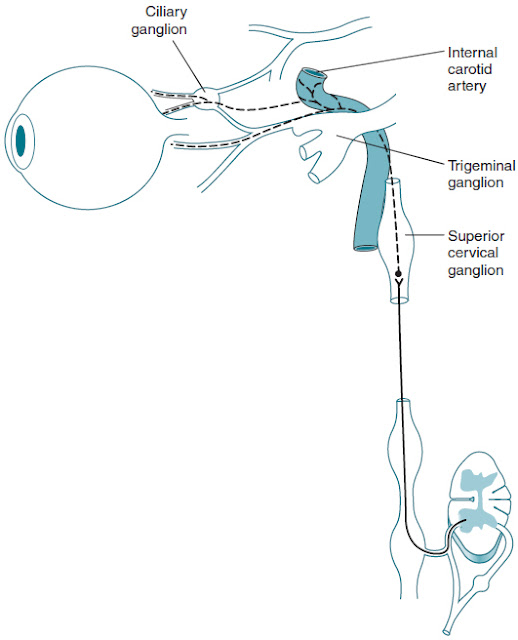
The sympathetic preganglionic neurons originate within the intermediolateral gray matter of the spinal cord, segments C8 to T2 (also known as the ciliospinal center of Budge-Waller), and receive indirect innervation from the ipsilateral hypothalamus. These preganglionic neurons exit the spinal cord via the dorsal roots and ascend in the sympathetic chain to synapse in the superior cervical ganglion in the distal neck. Postganglionic neurons then travel superficially on the internal and external carotid arteries. The axons on the external carotid artery innervate sweat glands in the skin, and the plexus on the internal carotid eventually joins the ophthalmic division of the trigeminal nerve. These fibers all pass through the ciliary ganglion without synapsing, enter the orbit with the nasociliary nerve, and innervate the dilator muscle via the long ciliary nerves (Figure 32–1).
Figure 32–1. Sympathetic nerve pathway of the eye.
Physical Examination
The first step in the pupillary examination is to note whether any anisocoria exists. If one pupil is smaller or larger than its counterpart, this can signify an autonomic nervous system disturbance. More specifically, an abnormally small pupil may signify a lesion in the sympathetic branch of the nervous system, while a large pupil may suggest a lesion affecting the parasympathetic branch. Pupil size should be assessed both in a well-lit room and a dark room. Worsening anisocoria in darkness suggests that the small pupil is the abnormal one because it is unable to dilate as well as the contralateral pupil to adjust to the darkness. Conversely, anisocoria that is more pronounced in the light suggests that the larger pupil is abnormal, as it is unable to constrict as well as the contralateral pupil in the presence of light. After assessing for anisocoria, it is important to observe the pupillary light reflex in each eye, both simultaneously and individually, using a strong light source. When light is shone in both pupils simultaneously, each should constrict to a similar degree.
While assessing pupils individually, each should constrict to direct as well as consensual stimulation in the contralateral eye.
If reaction to light is impaired, assess for intact accommodation by looking for pupillary constriction with near gaze. A pupil that accommodates but does not react is exhibiting a phenomenon called light-near dissociation. The final step in the pupillary examination is to perform the swinging-flashlight test to assess for presence of a relative afferent pupillary defect. When one eye has decreased afferent function relative to the other, the affected pupil will constrict when light is shone in the contralateral eye, but it will not constrict well in response to ipsilateral light stimulus. Because the affected eye is not sensing light properly, both pupils will appear to dilate when the light is swung toward the affected eye.
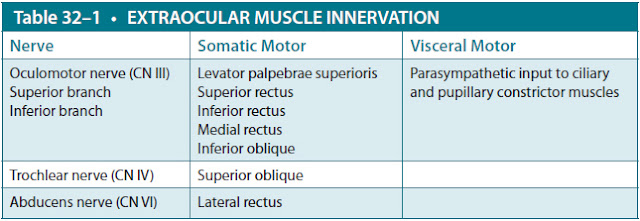
Extraocular motion is also an important part of the neuro-ophthalmic examination. Cranial nerves III, IV, and VI, as well as extraocular muscles, can be assessed by testing visual tracking in the six cardinal gaze directions. Recall that the lateral rectus is innervated by cranial nerve VI, the superior oblique is innervated by cranial nerve IV, and cranial nerve III supplies all other extraocular muscles, as well as the levator palpebrae superioris muscle. Parasympathetic fibers also travel with the inferior branch of cranial nerve III before they enter the ciliary ganglion (Table 32–1). The pattern of extraocular motor deficits combined with the pupillary examination and the rest of the cranial nerve examination, mental status, neck examination, and vitals can help localize and define the etiology of the lesion.
Differential Diagnosis
Third nerve palsy: The oculomotor nerve has multiple functions, as detailed in Table 32–1. A compressive lesion of the nerve will typically result in pupillary dilation as a result of parasympathetic fiber compression. Depending on the extent of compression, motor fibers may also be involved. When some function of the nerve remains, this is termed a “partial third nerve palsy.” When the entire nerve is compromised as in a “complete third nerve palsy,” the lesion is most likely microvascular. The most common third nerve compressive lesion is an aneurysm, usually of the posterior communicating or basilar arteries. While less common, the nerve can also be compressed by a tumor. In either case, third nerve compression can present as a “blown pupil,” which can be one of the first signs of impending uncal herniation. This would likely be associated with declining mental status and is a neurologic emergency.
CN, cranial nerve.
In this case, the patient’s pupillary dilation suggests parasympathetic involvement. The presence of multiple extraocular movement deficits and ptosis suggests that both branches of the nerve are compromised, likely from a lesion occurring proximal to their bifurcation. These findings are consistent with a partial third nerve palsy resulting from an aneurysm-related compression.
Horner syndrome is the presentation of ptosis, miosis, and anhidrosis that results from ipsilateral insult to the sympathetic pathway (runs from hypothalamus to the eye). Ptosis may be subtle and is a result of the paresis of Muller muscle. The palpebral fissure can also be diminished and is referred to as an “upside-down” ptosis of the lower lid. Anhidrosis occurs when the lesion is proximal to the carotid artery bifurcation and ipsilateral sweat glands are impaired. Miosis and “dilation lag” are a result of impaired sympathetic input to the pupillary muscles. This is especially evident after roughly 5 seconds in the dark, as the normal eye will already be fully dilated. However, after 12 to 15 seconds, the abnormal pupil will have slowly dilated to full diameter, decreasing the degree of anisocoria.
Congenital Horner syndrome can cause “heterochromia iridis,” a presentation where denervated areas of the iris remain lighter in color than the rest of the iris because sympathetic input is required for growth of the pigmented melanocytic cells. One iris may be a lighter color than that of the other eye, or a single iris may have areas of varied pigmentation.
Historically, cocaine drops were used to test for Horner syndrome due to the drug’s indirect sympathomimetic effects. In healthy patients, cocaine drops would cause a rapid dilation of the pupil, while patients with sympathetic lesions would exhibit no such response. Because cocaine is a controlled substance, apraclonidine is now used to assess suspected Horner syndrome. Apraclonidine is a weak alpha-1 agonist and a strong alpha-2 agonist. In a normal pupil, apraclonidine has only weak alpha-1 agonist activity and will cause no change of pupil size (due to dominating alpha-2 activity). However, patients with a lack of sympathetic input to the eye have an upregulation of alpha-1 adrenergic receptors on the dilator muscle, and as a result, they have a denervation hypersensitivity to alpha-1 agonists. Thus, when apraclonidine is applied to a patient with Horner syndrome, the eye is hypersensitive to the effects of the drug and exhibits dilation of the eye and reversal of anisocoria. Of note, apraclonidine only reverses the anisocoria if the lesion is a third-order neuron because first- and second-order neuron lesions do not leave the pupil dilator muscle denervated.
Pharmacologic anisocoria: There are multiple medications that can affect pupil size. Pilocarpine and organophosphates can both cause pupillary constriction, while medications such as atropine, tropicamide, and phenylephrine are routinely used to induce mydriasis in ophthalmology clinics. Similarly, scopolamine can also cause mydriasis, as can some plants. A detailed history that elicits potential exposures is key to the diagnosis of anisocoria, miosis, and mydriasis, and can help to avoid unnecessary and expensive workups for more serious intracranial lesions. For example, a patient may develop anisocoria after a breathing treatment if the face mask leaks on one side or if they touch their eye after touching their scopolamine patch (used for motion sickness, nausea, and hypersalivation).
Physiologic anisocoria, defined as a pupillary difference of 0.4 mm or more, is the most common cause of anisocoria, occurring in 20% of the general population. This phenomenon is speculated to be due to a sympathetic imbalance in innervation and is slightly more pronounced in the dark. The degree of anisocoria often changes over time and can even switch eyes. The condition is often a long-standing one that can be confirmed on review of old photographs. It is differentiated from Horner syndrome by the fact that there are no other associated symptoms, and there will never be dilation lag in the dark. No further evaluation is needed for this condition.
Light-near dissociation: Phenomenon in which pupils accommodate but have decreased or absent reaction to direct or consensual light. This can be caused by either optic neuropathy (ie, blindness), lesions of the dorsal midbrain (ie, Argyll Robertson pupil) or injury, and regeneration of oculoparasympathetic fibers (ie, tonic pupil). Optic neuropathy is the most common cause of light-near dissociation, as few light impulses reach the pretectal olivary nucleus; however, it is not often observed in clinic because accommodation is inconsistently assessed in blind patients. In patients with lesions of the dorsal midbrain (such as neurosyphillis), the light reflex pathway is interrupted, but the ventral fibers of the accommodation reflex are spared. Light-near dissociation in the setting of other neurologic symptoms is almost pathognomonic for Argyll Robertson pupil. Finally, in the setting of trauma or a compressive lesion, a light-near dissociation may develop as a result of aberrant regeneration of oculomotor nerve fibers (tonic pupil). Light-near dissociation can present as a component of various other syndromes, though less frequently than the above.
Tonic pupil (Adie pupil): Tonic pupil is characterized by poor or absent reaction to light, preserved accommodation on near gaze, and slowed/tonic redilation to near stimuli following constriction. This is due to postganglionic parasympathetic denervation of the sphincter muscle followed by aberrant reinnervation with accommodative fibers. Tonic pupil presenting with decreased deep tendon reflexes may be part of a syndrome known as Adie syndrome. A unilateral tonic pupil in an otherwise healthy individual is usually benign. Adie tonic pupils exhibit light-near dissociation in that accommodation is more pronounced than reaction to light. It can be distinguished from Argyll Robertson pupils by its sluggish reaction and its usual unilateral presentation (Argyll Robertson pupils are often bilateral).
Argyll Robertson pupil: A phenomenon associated with neurosyphilis, and a classic presentation of light-near dissociation where pupils will accommodate on near gaze but will not react to light. It can be differentiated from a tonic pupil in that the reactions are brisk instead of slow (or tonic). Argyll Robertson pupil has been attributed to lesions of the intercalated neurons in the midbrain or damage to inhibitory fibers of the oculomotor nucleus. It usually is a bilateral finding but may be asymmetric. The prevalence of Argyll Robertson pupils dropped significantly after the advent of penicillin therapy, but syphilis rates have risen in recent years.
Structural lesions: Congenital iris defects can lead to anisocoria. Acquired ocular lesions such as iris trauma (including surgery), inflammatory changes, or even angle-closure glaucoma can also cause pupil asymmetry. If an etiology is not clear in the history, an ophthalmologic examination should identify the cause.
Imaging
Any new-onset, complete or partial third nerve palsy with pupillary involvement is considered a neurologic emergency until proven otherwise, due to the possibility of aneurysm. Imaging must be performed immediately. Imaging should also be performed in patients who are younger than 50 years, have a history of cancer, have other neurologic signs or symptoms, or who have no resolution of a suspected microvascular ischemic neuropathy after 3 months. The gold standard to assess for an aneurysm is still 4 vessel catheter angiogram; however, most patients will receive noninvasive imaging with a CT/CT angiogram (CTA) or MRI/MRA first. MRA and CTA each have a small number of false-negative studies, but the combination of MRI/MRA/CTA approaches 100%.
CASE CORRELATION
- See also Case 23 (Optic Neuritis)
COMPREHENSION QUESTIONS
32.1 to 32.4. Match the following (A to G) to the clinical scenario.
A. Third nerve palsy
B. Horner syndrome
C. Pharmacological effect
D. Physiologic anisocoria
E. Argyll Robertson pupils
F. Tonic pupil
G. Structural defect
32.1 A 32-year-old man presents with anisocoria and mild left ptosis 2 days after being in a motor vehicle accident. Apraclonidine drops applied to the left eye reverse the anisocoria.
32.2 A 58-year-old pharmacy technician presents to the emergency department after her shift because she noticed that her right pupil is much larger than her left pupil. She denies any other symptoms.
32.3 A 54-year-old man with large right middle cerebral hemisphere stroke 1 day ago admitted to the intensive care unit (ICU) for monitoring is noted to be lethargic. His right pupil appears larger and less briskly reactive than the contralateral pupil.
32.4 A 27-year-old woman presents to clinic for evaluation of her migraine headaches. She is noted to have 0.5-mm asymmetry of the pupils, but both react well to light and accommodate. She has no other neurologic deficits.
32.5 Which of the following patients is at the least risk for a life-threatening intracranial process and could be observed without imaging?
A. A 48-year-old man with history of diabetes, hypertension, and hyperlipidemia who presents with an enlarged right pupil, right-sided ptosis, and diplopia.
B. A 67-year-old man with a history of diabetes and hypertension who presents with diplopia, inferolateral eye deviation, and significant ptosis.
C. A 77-year-old man with a history of diabetes, lung cancer, and a seizure 2 months ago who presents with a partial third nerve palsy.
D. A 72-year-old woman with history of diabetes, hypertension, and polymyalgia rheumatica with third nerve palsy diagnosed 4 months ago who returns to clinic without any sign of improvement.
32.6 A 24-year-old woman with a visual disturbance is being evaluated by her physician. The physician is concerned about a possible sympathetic lesion affecting the right eye. Which of the following evaluations is most likely to uncover this lesion?
A. Check for pupillary constriction in light.
B. Check for pupillary dilation in dark.
C. Check for upward eye gaze.
D. Check for lateral eye gaze.
E. Check for medial eye gaze.
F. Check for accommodation.
ANSWERS
32.1 B. This man most likely has Horner syndrome induced by a carotid dissection. The apraclonidine confirms the third-order sympathetic neuron lesion. He needs angiographic evaluation of the neck vasculature.
32.2 C. Pharmacologic anisocoria is strongly suspected in this patient due to her risk of workplace exposure to mydriatic agents. Depending on the rest of her history and examination, she likely can be safely discharged without extensive workup.
32.3 A. Third nerve palsy. This patient is at risk for cerebral edema due to his large stroke. Because he is relatively young, he will have less brain atrophy and therefore less room to accommodate swelling within the cranium than would an elderly patient. The mass effect causes downward herniation of the uncal portion of the temporal lobe, compressing the third nerve in the process. He needs emergent CT and neurosurgical consultation for possible hemicraniectomy.
32.4 D. Physiologic anisocoria is the most common cause of pupil asymmetry. It is often small (<0.4 mm), and the pupils should otherwise react normally. This is unlikely to be related to her migraines, although a small number of patients may experience anisocoria with their headaches due to altered sympathetic function.
32.5 B. All four patients have a third nerve palsy. An older individual (>age 50) with vascular risk factors and no other symptoms is likely suffering from a microvascular ischemic lesion in the deep fibers of the third nerve. This condition almost always resolves within 3 months and can often be observed for a time before proceeding with imaging. Poor resolution of symptoms over time, however, would decrease the likelihood of microvascular ischemic neuropathy, and further workup would be recommended. Patients who are younger, have a history of cancer, or have any other neurologic symptoms need imaging. Imaging should be performed in patients with pupil involvement, partial nerve palsy, or with poor resolution. The 48-year-old man is rather young for an ischemic neuropathy, and pupil involvement is less common with microvascular insults. A new cranial nerve lesion in a 77-year-old man with a history of lung cancer and recent seizure raises concern for metastatic disease. Cranial neuropathy may be a presenting sign of giant cell arteritis in a subset of patients, and polymyalgia rheumatica has a strong association with this vasculitis.
32.6 B. Sympathetic lesions will also cause abnormal constriction of the pupil, which will be most obvious in the dark because the impaired pupil will dilate much more slowly. However, after waiting 12 to 15 seconds, the pupil will reach its final diameter, and the anisocoria will be less apparent. Sympathetic lesions do not affect extraocular movements or accommodation.
CLINICAL PEARLS
|
▶ A third nerve palsy involving the
pupil is considered a medical emergency, as it may be a sign of an
intracranial aneurysm (most commonly of the posterior communicating artery or
basilar artery).
▶ Aneurysm is the most common
compressive cause of an isolated oculomotor nerve palsy.
▶ When anisocoria is identified,
additional examination findings such as ptosis and extraocular motion
deficits can help determine which pupil is abnormal.
▶ Sympathetic lesions will be more
obvious in the dark and will localize to the smaller pupil. Parasympathetic
lesions will be more apparent in the light and localize to the larger pupil.
▶ Physiologic anisocoria is the most
common cause of asymmetric pupils.
|
REFERENCES
Bruce BB, Biousse V, Newman NJ. Third nerve palsies. Semin Neurol. 2007;27(3):257-268.
Colby K. Anisocoira. The Merck Manual Professional Edition. 2014 Aug. http://www.merckmanuals.
com/professional/eye_disorders/symptoms_of_ophthalmologic_disorders/anisocoria.html. Accessed February 16, 2015.
Cooper-Knock J, Pepper I, Hodgson T, Sharrack B. Early diagnosis of Horner syndrome using topical apraclonidine. J Neuroopthalmol. 2011;31(3):214-216.
Dorland’s Illustrated Medical Dictionary. 27th ed. Philadelphia, PA: WB Saunders; 1988.
Kawasaki A. Physiology, assessment, and disorders of the pupil. Curr Opin Ophthalmol. 1999;10(6):
394-400.
Kawasaki AK. Diagnostic approach to pupillary abnormalities. Continuum (Minneap Minn). 2014;
20(4 Neuro-ophthalmology):1008-1022.
Kedar S, Biousse V, Newman NJ. Approach to the patient with anisocoria. UpToDate. 2014 Jan. http://www.uptodate.com/contents/approach-to-the-patient-with-anisocoria. Accessed February 16, 2015.
Loewenfeld IE. The Pupil: Anatomy, Physiology and Clinical Applications. Ames, IA: Iowa State University Press and Detroit, MI: Wayne State University Press; 1993.
Murchison AP, Gilbert ME, Savino PJ. Neuroimaging and acute ocular motor mononeuropathies: a prospective study. Arch Ophthalmol. 2011;129(3):301-305.
Wilhelm H. Disorders of the pupil. Handb Clin Neurol. 2011;102:427-466.
Wilson-Pauwels L, Akesson EJ, Stewart PA. Cranial Nerves: Anatomy and Clinical Comments. Philadelphia, PA: B.C. Decker; 1988.

0 comments:
Post a Comment
Note: Only a member of this blog may post a comment.