Pseudotumor Cerebri/Idiopathic Intracranial Hypertension Case File
Eugene C. Toy, MD, Ericka Simpson, MD, Pedro Mancias, MD, Erin E. Furr-Stimming, MD
CASE 33
A 26-year-old obese woman presents to the emergency room with a severe headache and blurred vision. She has been experiencing headaches over the past 2 to 3 weeks. Her headaches are described as an aching sensation encompassing the entire head. She has been able to remain functional until today, when the severity of the headache acutely worsened to the point she could not tolerate it. She has taken acetaminophen without improvement in her symptoms. She has not experienced nausea, vomiting, or any other symptoms besides visual impairment. Over the past 2 weeks, she has experienced transient graying out of her vision, most noticeably when she gets up from a chair. Her temperature is 37.2°C (98.9°F), blood pressure 134/72 is mm Hg, heart rate is 78 beats/min, weight is 108.8 kg (240 lb), and height is 155 cm (5 ft 1 in). As the emergency room physician, you notice the following on examination: there are no cranial bruits, and her cardiovascular examination is normal. Her neurologic examination is notable for bilateral disc edema with intact visual acuity and full extraocular muscle movements. Her visual fields are normal on bedside confrontation examination. The remainder of her neurologic examination, including mental status, is completely normal. A comprehensive metabolic panel, complete blood count (CBC), urinalysis, and computed tomography (CT) scan of the head are all normal.
▶ What is the most likely diagnosis?
▶ What is the next diagnostic step?
▶ What is the next step in therapy?
ANSWERS TO CASE 31:
Pseudotumor Cerebri/Idiopathic Intracranial Hypertension
Summary: A 26-year-old obese woman presents with blurred vision and a severe headache. She provides a history of experiencing transient graying out of her vision over the past 2 to 3 weeks. She has no other associated symptoms. Her physical examination is notable for bilateral papilledema and obesity. The serum laboratory tests, urinalysis, and CT scan of the head are normal.
Most likely diagnosis: Increased intracranial pressure.
Next diagnostic step: Emergent CT imaging followed by lumbar puncture
(if safe), and ophthalmic evaluation with formal visual field testing.
Next step in therapy: A lumbar puncture is the first step in therapy in the acute setting.
- Describe the diagnostic approach to pseudotumor cerebri.
- Describe the differential diagnosis of papilledema.
- Be familiar with emergent treatment of elevated intracranial pressure.
Considerations
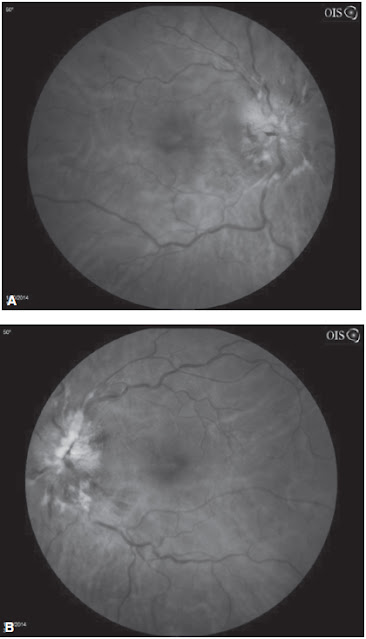
The presentation of headache with blurred vision and papilledema is a medical emergency. Papilledema denotes a serious neurologic problem and most commonly occurs bilaterally. When acute, vision for the most part is well preserved. Papilledema is defined as swelling of the optic disc from elevated intracranial pressure (Figure 33–1). It can be a sign of an underlying brain mass, which, even if benign, can cause increased intracranial pressure, placing patients at risk for irreversible neurologic dysfunction or even death. Depending on the size of the brain mass and the extent of its associated edema, patients are at risk for herniation syndromes, which eventually can lead to death. In general, all patients with increased intracranial pressure with papilledema require emergent neuroimaging studies. The study of choice in emergent situations remains a CT scan of the head with contrast. Conditions that can cause papilledema include meningitis, hydrocephalus, space-occupying lesions, dural sinus thrombosis, and pseudotumor cerebri (also known as idiopathic intracranial hypertension). Pseudotumor cerebri is a diagnosis of exclusion. It tends to affect women of childbearing age, and affected women are often obese.
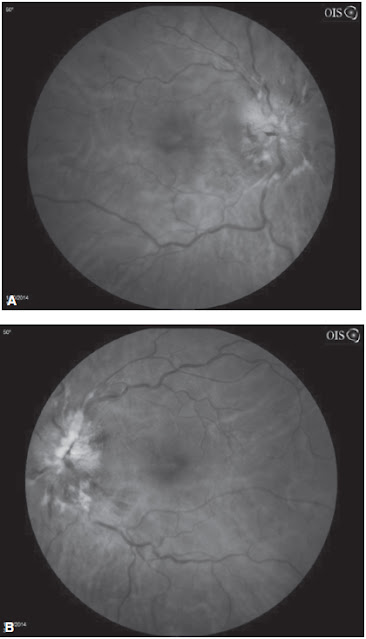
Figure 33–1. Fundus photographs from a patient with bilateral papilledema due to pseudotumor cerebri. A is the right eye and B is the left eye. (Reproduced, with permission, from Sushma Yalamanchili, MD.)
DEFINITIONS
PAPILLEDEMA: Disc edema from raised intracranial pressure, commonly bilaterally.
HYDROCEPHALUS: Abnormal excessive accumulation of cerebrospinal fluid (CSF) in the brain.
LUMBAR PUNCTURE: A test that evaluates CSF and opening pressure. It is performed under local anesthesia and involves placing a needle into the spinal canal, typically at L4-L5, for collection of spinal fluid.
CLINICAL APPROACH
Pathophysiology
Papilledema results from axoplasmic flow stasis in the slow axoplasmic transport system. Increased intracranial pressure is transmitted to the subarachnoid space, which in turn encompasses the entire optic nerve and is continuous with the optic nerve sheath. As intracranial pressure increases, the pressure in this sheath also increases, resulting in a blockage at the nerve and preventing normal axoplasmic transport. The collection of components involved in axonal transport leads to marked distension of optic axons, which in turn results in edema of the nerve and optic disc. Disc edema can be caused from many different etiologies, including inflammation, tumors, infections, and ischemia. However, papilledema refers only to the disc edema caused by increased intracranial pressure.
Evaluation
The finding of papilledema on clinical examination in the setting of recent neurologic symptoms such as headaches or visual disturbances should alert the clinician of a possible space-occupying lesion in the brain. The history and physical examination can sometimes help localize a mass lesion. For example, right-sided weakness associated with headaches, papilledema, and visual disturbances would place the mass lesion in the left cerebral hemisphere. However, the etiology of this space-occupying lesion cannot be determined by examination alone. In the emergent setting, a CT scan of the head with and without contrast is helpful in trying to determine if this mass lesion is a tumor, hemorrhage, abscess, and so forth. Importantly, it will assist in diagnosing associated cerebral edema and impending cerebral herniation. When time allows, magnetic resonance imaging (MRI) of the brain with and without contrast provides greater detail to assess for tumors or infections. An MR venogram can exclude a dural venous sinus thrombosis.
In the absence of a mass lesion, a lumbar puncture is the next step to evaluate the cause of increased intracranial pressure. Opening pressure of the CSF is measured and recorded with the patient in the recumbent position. Lumbar punctures performed in an upright position do not allow for accurate pressure measurements. If the CSF pressure is elevated greater than 20 cm of water, the clinician can choose to remove a large amount of CSF (>40 mL), otherwise known as a high-volume tap. The CSF should be sent for culture and analyzed for protein, glucose, cell count with differential, immunoglobulin G (IgG) synthesis panel, and cytology. Additionally, a note should be made of the color and clarity of the fluid. This analysis will help evaluate for conditions such as meningitis or other infections, hemorrhage, or inflammation.
Visual disturbances can become permanent if the edema persists, as patients experience a progressive loss of peripheral vision. All patients need a formal ophthalmologic examination, including visual field testing, in addition to their neurologic evaluation.
PSEUDOTUMOR CEREBRI
Epidemiology
Pseudotumor cerebri also is referred to as idiopathic intracranial hypertension or benign intracranial hypertension. It is often seen in young obese women and has an incidence rate in the United States of approximately 1 per 100,000 in the general population. The incidence is slightly higher in women who are overweight. The diagnosis is one of exclusion and requires the findings of increased intracranial pressure (papilledema), nonfocal neurologic signs (with the exception of a possible sixth cranial nerve palsy), normal imaging studies (except for slit-like ventricles), and normal CSF studies except for an elevated opening pressure. Although this can present at any age, most patients present in the third decade of life.
Pathophysiology
The pathophysiology of pseudotumor cerebri is unclear; however, it is presumed that there is a resistance to absorption of CSF across the arachnoid villi. Others believe that the cerebral circulation is abnormal and that cerebral venous outflow is impaired, which results in increased water content in the brain. It has been suggested that obesity leads to increased intra-abdominal pressure, which raises cardiac filling pressures, which in turn leads to impaired venous return from the brain. This leads to an elevation in intracranial venous pressure. Whatever the cause, the resultant increased intracranial pressure is relayed to anatomic structures in the brain cavity, resulting in neurologic signs and symptoms.
Clinical Evaluation
Typical symptoms for pseudotumor cerebri include headache, transient visual obscuration, dizziness, nausea, vomiting, pulsatile tinnitus, and horizontal diplopia from a sixth nerve palsy. The classic headache associated with pseudotumor cerebri is diffuse, worsens in the morning, and worsens by Valsalva maneuver. Patients often report transient visual obscuration or graying out/dimming of vision that is exacerbated after bending over or standing up quickly. The most common abnormality on clinical examination is bilateral disc edema. Disc edema can be asymmetric, and there can be associated subretinal hemorrhages. If untreated, it can lead to irreversible optic nerve damage.
Risk factors for pseudotumor cerebri include obesity, recent weight gain, female gender, being in the reproductive age group, and menstrual irregularity. Some cases have been associated with hypothyroidism, Cushing disease, adrenal insufficiency, chronic renal failure, systemic lupus erythematosus, lithium, tamoxifen, tetracycline, cimetidine, and retin-A–containing medications. Discontinuation of corticosteroids has also been associated with the development of pseudotumor cerebri.
In the evaluation process, imaging studies should be performed to exclude mass lesions, infections, hemorrhage, and dural venous sinus thrombosis. Typically, neuroimaging studies are normal in patients with pseudotumor cerebri. However, enlarged optic nerve sheaths, flattening of the posterior portion of the globe, small slit-like ventricles, or an empty sella may be seen. If imaging studies are normal, a lumbar puncture is performed to evaluate opening pressure. CSF studies as described earlier should be performed. In pseudotumor cerebri, all CSF studies should be normal, except for an elevated opening pressure. Additionally, visual fields should be evaluated by an ophthalmologist to clearly document any subtle abnormalities. The presence of objective deficits on formal examination can significantly impact the treatment plan.
Treatment
Treatment of pseudotumor cerebri includes a high-volume lumbar puncture performed at the time of the initial evaluation. This, however, is only temporary. Long-term treatment includes the use of a carbonic anhydrase inhibitor such as acetazolamide or topiramate, which lowers the intracranial pressure through decreased CSF production. In addition, these medications have a side effect of weight loss that can be beneficial in these patients. Furosemide has also been used alone and in combination with carbonic anhydrase inhibitors. If the patient is experiencing significant or progressive visual loss, the next step is to perform optic nerve sheath fenestrations. This involves cutting patches in the dura surrounding the optic nerve, allowing efflux of CSF, which in turn reduces pressure. If medical management is insufficient, a lumbar peritoneal shunt or ventriculoperitoneal shunt is performed by neurosurgeons. Weight reduction is essential to the long-term management of the disease, and bariatric surgery may need to be considered in some patients.
COMPREHENSION QUESTIONS
33.1 An emergency room physician has found what appears to be papilledema on examination in a 40-year-old woman. The intracranial pressure is noted to be normal. Which of the following conditions is most likely to be causative?
A. Metastatic breast cancer
B. Intracerebral hemorrhage
C. Hydrocephalus
D. Idiopathic intracranial hypertension
E. Optic nerve trauma
33.2 Which of the following is a risk factor for pseudotumor cerebri or idiopathic intracranial hypertension?
A. Thin physique
B. Hyperthyroidism
C. Recent weight loss
D. Female gender
33.3 A 25-year-old woman with recent weight gain presents with headaches. She is diagnosed with pseudotumor cerebri. Other than mild papilledema, her examination is normal. Which of the following is the best next step in therapy?
A. Acetazolamide
B. Optic nerve sheath fenestration
C. Lumbar peritoneal shunt
D. Bariatric surgery
ANSWERS
33.1 E. The physician is observing findings suggestive of papilledema such as swelling of the optic margins and elevation of the optic disc. In this patient, the intracranial pressure has been measured and is normal; thus, the optic nerve disc findings is not due to a “pressure” process. Optic nerve trauma can cause the swelling and optic nerve changes. It is not due to intracranial pressure and thus is not referred to as papilledema. In summary, all the answer choices are options that can cause optic disc edema, but optic nerve trauma was the only option that would not be secondary to increased intracranial pressure.
33.2 D. Female gender places the patient at higher risk for benign intracranial hypertension.
33.3 A. Acetazolamide decreases the intracranial pressure and would be a good initial treatment option for this patient. Many pseudotumor cerebri patients do undergo shunt placement, but only if they do not tolerate or respond to medical management. Optic nerve sheath fenestration would only be indicated if she were having rapid and/or progressive visual loss. Bariatric surgery should only be considered in obese patients who fail to lose weight by diet and exercise. Medical management should always be attempted before invasive surgical options unless there is an emergent indication (eg, rapid visual loss).
CLINICAL PEARLS
|
▶ “Papilledema” is a term that should
only be used for optic disc swelling secondary to increased intracranial
pressure.
▶ Papilledema associated with visual
dysfunction is a medical emergency requiring immediate neuroimaging studies.
▶ The neurologic examination in
patients with pseudotumor cerebri should be normal except for papilledema,
visual loss, and a possible sixth nerve palsy.
▶ Lumbar puncture can be both
diagnostic and therapeutic in patients with pseudotumor cerebri.
▶ Acute treatment of pseudotumor cerebri
includes a high-volume lumbar puncture, followed by long-term treatment with
a carbonic anhydrase inhibitor such as acetazolamide or topiramate.
|
REFERENCES
Brazis PW, Lee AG. Elevated intracranial pressure and pseudotumor cerebri. Curr Opin Ophthalmol. 1998;9(6):27-32.
Green MW. Secondary headaches. Continuum (Minneap Minn). 2012;18(4):783-795.
Miller NR, Newman NJ. Pseudotumor cerebri (benign intracranial hypertension). In:
Miller NR, Newman NJ, Biousse V, et al, eds. Walsh and Hoyt’s Clinical Neuro-Ophthalmology, Vol. 1. 6th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2004:523-538.
Pham L, Wall M. Idiopathic intracranial hypertension (pseudotumor cerebri). University of Iowa Ophthalmology and Visual Sciences website. Updated February 2, 2010. http://webeye.ophth.uiowa.edu/eyeforum/cases/99-pseudotumor-cerebri.htm. Accessed February 15, 2015.

0 comments:
Post a Comment
Note: Only a member of this blog may post a comment.