Sixth Nerve Palsy (Ischemic Mononeuropathy) Case File
Eugene C. Toy, MD, Ericka Simpson, MD, Pedro Mancias, MD, Erin E. Furr-Stimming, MD
CASE 34
A 65-year-old man with a history of hypertension, coronary artery disease, and diabetes mellitus presents with a complaint of double vision that started yesterday. He has not experienced any other general or neurologic symptoms. He noticed covering up either eye corrects his double vision, and has resorted to wearing an eye patch since yesterday so that he can see and walk without falling. In fact, he was able to drive on his own on the freeway to your office, much to his family’s dismay. On further questioning, you elicit the history that his double vision is worse when he looks to the right and better with gaze to the left. He has been compliant with his medications for hypertension and coronary artery disease. On examination, his blood pressure is 124/72 mm Hg, with a heart rate of 88 beats/min. He is afebrile and has a regular rate and rhythm without murmurs on cardiac examination. There are no carotid bruits, and his peripheral pulses are normal. His neurologic examination is notable for intact orientation and intact motor strength. His cranial nerve examination is remarkable only for impaired abduction of the right eye. Sensory examination is normal, and his deep tendon reflexes are 2+ throughout. Plantar responses are downgoing. His gait is normal. Review of his daily blood pressure log shows stable pressures around 130/70 mm Hg.
▶ What is the neurologic deficit?
▶ What is the most likely diagnosis?
ANSWERS TO CASE 34:
Sixth Nerve Palsy (Ischemic Mononeuropathy)
Summary: A 65-year-old man with hypertension, coronary artery disease, and diabetes mellitus presents with a 24-hour history of binocular horizontal diplopia (double vision). He has not experienced associated symptoms such as headache. His examination is significant for a normal blood pressure and heart rate and the findings of the isolated right sixth nerve palsy.
- Likely neurologic deficit: Sixth nerve palsy
- Most likely diagnosis: Ischemic mononeuropathy
- Understand the diagnostic approach in evaluating diplopia.
- Describe the difference between monocular and binocular diplopia.
- Know the differential diagnosis of a sixth nerve palsy.
Considerations
This 65-year-old man with known risk factors for cerebrovascular disease (hypertension, diabetes, and coronary artery disease) presents with an acute episode of binocular diplopia. The history suggests binocular diplopia, as he tells you that covering up an eye resolves the diplopia. You are given the history that he has diplopia only on horizontal gaze. Given the history of hypertension and coronary artery disease, he is at risk for cerebrovascular disease and ischemia. In this particular case, you are told that the patient’s brain magnetic resonance imaging (MRI) is normal. In this setting, the most likely cause of diplopia is microvascular ischemic mononeuropathy of the peripheral abducens nerve.
APPROACH TO:
Binocular Diplopia
DEFINITIONS
DIPLOPIA: Double vision.
ISCHEMIC MONONEUROPATHY: Isolated nerve injury from inadequate blood flow to the nerve.
PTOSIS: Drooping of the eyelid.
Sixth nerve or abducens nerve palsy has a variety of causes, and a detailed history and clinical examination usually lead to an accurate diagnosis. Unilateral abducens palsy is the most common isolated ocular motor palsy. A careful review of the anatomic course of the abducens nerve can help delineate the location of the lesion.
The abducens nucleus is located in the lower dorsal pons. The motor neurons of this nucleus send axons that course anteriorly in the pons and travel near the corticospinal tract and emerge in the sulcus between the pons and medulla. The abducens nerve exits the pons ventrally and ascends in the prepontine cistern via the subarachnoid space. It pierces the dura lateral to the dorsum sellae of the sphenoid bone. It then rises over the petrous apex of the temporal bone and enters the cavernous sinus lying between the carotid artery and the ophthalmic branch of the trigeminal nerve laterally. It finally passes through the medial end of the superior orbital fissure and through the tendinous ring to enter the deep surface of the lateral rectus muscle.
Etiology of Sixth Nerve Palsy
After the localization of the lesion to the sixth cranial nerve, the next step is to determine the etiology of the abnormality. Vascular lesions are a common cause of sixth nerve palsy. An infarct in the basal pons can also damage the nucleus or the axons, as these travel toward the ventral surface from the nerve. Microvascular ischemia can occur at any point along the nerve’s path and may be painful. Posterior inferior cerebellar artery or basilar artery aneurysms may also compress the nerve. Masses in the fourth ventricle, skull base, and cavernous sinus can also compress the nerve. Inflammatory and infectious processes may also affect the nerve (eg, sarcoidosis, extension of a middle ear infection). It is also prone to injury with fractures of the skull base. The sixth cranial nerve is most commonly affected by elevated intracranial pressure due to impingement over the petrous temporal ridge. This is considered a “false localizing sign” because the nerve palsy suggests a focal lesion when the true problem is often diffuse elevation of intracranial pressure, and the underlying cause of the elevated pressures may or may not localize to the same side as the sixth nerve palsy.
Evaluation of Diplopia
Diplopia results from lack of visual fusion. The first step in evaluating a patient with diplopia is to determine whether it is binocular or monocular. Binocular diplopia denotes double vision arising from misalignment of both the eyes and is caused by an underlying primary neurologic problem. Covering up either eye resolves the double vision. Monocular diplopia is primarily caused by an ophthalmologic disorder such as abnormalities of the lens, cornea, or vitreous humor. Only rarely is monocular diplopia caused by occipital lobe disease or seizures. Monocular diplopia arises from a primary problem within one eye and does not resolve when an eye is covered.
The next step in evaluating someone with binocular diplopia is to determine if it is horizontal or vertical. Different eye muscles are involved in moving the eyes horizontally or vertically. There are only two muscles in each eye responsible for horizontal gaze, and those are the medial rectus (innervated by the third nerve) and the lateral rectus (innervated by the sixth nerve). Worsening horizontal diplopia on near vision could suggest a problem with the medial rectus, whereas horizontal diplopia that worsens when viewing distant and lateral objects could indicate a problem with the lateral rectus.
Examining extraocular muscles in the six cardinal fields of gaze can readily point out which of the two muscles is affected. For example, if the right eye cannot cross the midline and look out laterally, the lateral rectus is affected. Conversely, if the right eye cannot cross the midline and turn inward, the medial rectus is affected. The red lens test can help determine which eye muscle is causing the diplopia. A red lens is placed over the right eye, and the patient is asked to follow the movements in six positions of cardinal gaze. The key to performing this test is to understand the following: (1) Image separation will be greatest in the direction of the weak muscle, and (2) the image that is the farthest away from the midline is a false image and corresponds to the eye with impaired motility.
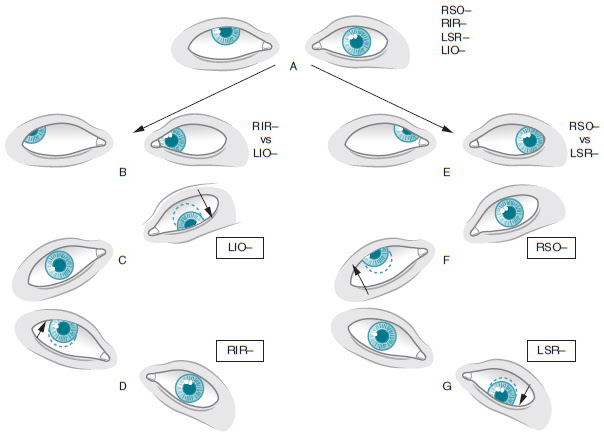
The other four eye muscles (superior rectus, inferior rectus, inferior oblique, and superior oblique) move the eyes vertically. Individuals that present with vertical binocular diplopia are experiencing weakness in one or several of these muscles. Vertical diplopia that worsens on near vision suggests a problem with either the inferior oblique or superior oblique. A fourth nerve palsy will have worse diplopia on downward gaze. The three-step Parks-Bielschowsky test can be used to localize the impaired muscle causing vertical diplopia. Each step assesses whether the dysconjugate gaze is worse in a particular direction. First, determine which eye is hypertrophic (elevated or “higher up” compared to the other) on primary midline gaze. If the right eye appears higher than the left, this means the right eye depressors (right inferior rectus, right superior oblique) or the left eye elevators (left superior rectus, right inferior oblique) are weak. The second step assesses whether the hypertropia increases on right or left gaze. The vertical rectus muscles have their greatest vertical action when the eye is abducted and the oblique muscles have their greatest vertical action when the eye is adducted. In the final step, determine whether the hypertropia increases on right or left head tilt. For example, a right fourth nerve palsy would have right eye hypertropia on primary gaze. The hypertropia and diplopia would be worse on left gaze and right head tilt. Left head tilt would help the diplopia, and the patient may naturally assume that position (Figure 34–1). A red lens test may be performed in conjunction with this test. Another option is to use a Maddox rod, a more advance form of red lens testing.
Evaluating other aspects of the cranial nerve examination may also help localize the lesion. Special attention should be given to the eyelid, pupillary responses, symmetry of the pupillary size, and abnormalities of cranial nerves V, VII, and VIII. For example, ptosis or droopiness of the eyelid can suggest a third nerve problem. Likewise, pupillary asymmetry suggests a third nerve problem. Multiple cranial nerve involvement may indicate a lesion in the brainstem, cavernous sinus, or orbit, depending on the particular nerve’s involvement. Variable fatigability of the eyelid can suggest myasthenia gravis.
The evaluation includes serologic studies including an erythrocyte sedimentation rate (ESR), C-reactive protein (CRP), antinuclear antibody (ANA), complete blood count (CBC), and hemoglobin A1c. An ESR, CRP, and ANA can help exclude inflammatory causes such as vasculitis; glycosylated hemoglobin can exclude diabetes mellitus, and a CBC can exclude infectious processes. An MRI of the brain and orbits can exclude vascular abnormalities such as an aneurysm and can exclude lesions that are inflammatory (sarcoid), demyelinating, neoplastic, or due to brainstem infarct. Imaging of the brain and vasculature must be considered in suspected third cranial nerve palsies, especially if the pupil is involved, due to the possibility of compression of the peripherally lying parasympathetic fibers by a posterior communicating artery aneurysm. Ancillary studies such as cerebrospinal fluid (CSF) analysis may be necessary in younger patients if imaging is inconclusive. Most clinicians will also obtain imaging in patients with isolated fourth or sixth nerve palsies. An ischemic process may not be readily visualized on imaging studies and is often a diagnosis of exclusion.
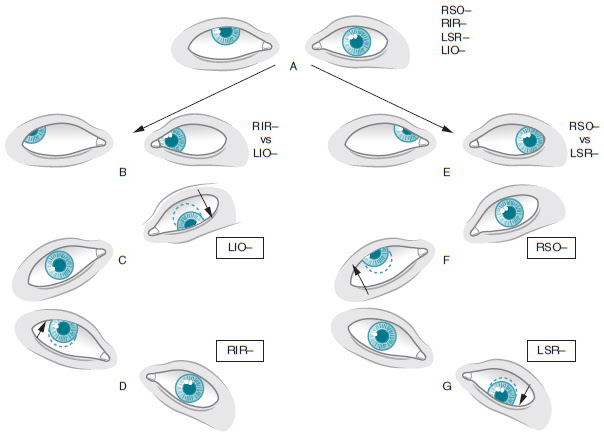
Figure 34–1. Example of the three-step Parks-Bielschowsky test. LSO/RSO, left/right superior oblique; LIO/RIO, left/right inferior oblique; LSR/RSR, left/right superior rectus. (Reproduced, with permission, from von Noorden GK. Atlas of Strabismus. 4th ed. St Louis, MO: Mosby-Year Book; 1983.)
TREATMENT
Treatment is focused on symptomatic relief and controlling the underlying medical conditions, particularly diabetes. An isolated and presumed ischemic-related sixth nerve palsy can be observed for improvement for 1 to 3 months. Patching of the involved eye can help alleviate diplopia symptoms temporarily. Eyeglasses made with prism lens can also be used to minimize or correct diplopia during recovery. Some suggest using botulinum toxin as a temporizing measure. It is injected into the antagonist muscle of the paretic muscle and the effect of a single injection can last for up to 3 to 6 months. If these measures fail, strabismus surgery on the extraocular muscles to try to correct the misalignment may be of benefit in some patients. Surgery should not be considered until adequate time has been given for recovery.
CASE CORRELATION
- See also Case 24 (Multiple Sclerosis) and Case 32 (Posterior Communicating Artery Aneurysm)
COMPREHENSION QUESTIONS
34.1 Which of the following is most accurate regarding diplopia?
A. Binocular diplopia refers to double vision occurring from intrinsic problems in both eyes.
B. Monocular diplopia most commonly occurs because of extrinsic eye problems.
C. On red lens testing, the false image is always the image closest to the midline.
D. The key in evaluating diplopia is to start by determining if it is monocular or binocular.
34.2 A 33-year-old woman has a 3-minute seizure episode caused by her epilepsy. There are no underlying medical disorders or brain structural lesions. Which of the following indicates a more complicated underlying neurologic problem?
A. Urinary incontinence with seizure
B. Confusion and lethargy after seizure
C. Headache after the seizure
D. Sixth nerve palsy after seizure
34.3 A 58-year-old woman suffers from an ischemic-related sixth nerve palsy, which occurred 6 months ago. Various methods have been tried with limited success, and the patient still has diplopia. Which of the following is most likely to be helpful at this stage?
A. Surgery
B. Eye patch
C. Prisms
D. Prednisone at a dose of 10 mg/d
ANSWERS
34.1 D. The key to evaluating diplopia is to assess unilateral versus bilateral. In most cases, binocular diplopia arises from a primary neurologic problem and monocular diplopia is due to a primary ophthalmologic issue. The false image on red lens testing is always the farthest from the midline.
34.2 D. Seizures have not been reported to cause sixth nerve dysfunction, and thus its presence indicates a more complex situation such as space-occupying lesion. A sixth nerve palsy can be a sign of elevated intracranial pressure. Headache, postictal confusion and lethargy, and incontinence are commonly associated with seizures.
34.3 A. Surgery may be considered in patients with persistent symptoms that have not resolved and are not controlled by less invasive methods. Surgery is not considered immediately, as many patients will recover function within a few months. Prednisone has not been used for sixth nerve palsies from ischemia but can be used for inflammatory causes of sixth nerve abnormalities.
CLINICAL PEARLS
|
▶ Localization of diplopia can be
determined with careful interview and clinical examination. It is essential
to determine if the diplopia is (1) binocular or monocular and (2) horizontal
or vertical.
▶ Binocular diplopia typically occurs
from misalignment of the eye muscles on a target and commonly denotes an
underlying primary neurologic problem. Monocular diplopia results from
intrinsic eye problems.
▶ MRI of the brain should be considered
when evaluating patients with binocular diplopia, as it allows for the
detection of vascular or demyelinating processes and mass lesions.
▶ Isolated cranial nerve palsies are
often due to microvascular ischemia, especially in older patients with
vascular risk factors such as diabetes mellitus.
▶ A sixth nerve palsy can be a sign of
increased intracranial pressure but it does not necessarily help localize the
causative lesion.
▶ A third nerve palsy involving the
pupil (pupil dilation) is considered a medical emergency, as it may be a sign
of a posterior communication artery aneurysm.
|
REFERENCES
Cybersight by Project Orbis International Inc. Parks-Bielschowsky Test. http://www.cybersight.org/bins/content_page.asp?cid=735-2858-4397-4781-5287-5289-5292. Accessed February 15, 2015.
Danchaivijitr C, Kennard C. Diplopia and eye movement disorders. J Neurol Neurosurg Psychiatry. 2004;75:iv24-iv31.
Patel SV, Mutyala S, Leske DA, Hodge DO, Holmes JM. Incidence, associations, and evaluation of sixth nerve palsy using a population-based method. Ophthalmology. 2004;111:369-375.
Quah BL, Ling YL, Cheong PY, Balakrishnan V. A review of 5-years’ experience in the use of botulinum toxin A in the treatment of sixth cranial nerve palsy at the Singapore National Eye Centre. Singapore Med J. 1999;40:405-409.
Savino PJ. Diplopia and sixth nerve palsies. Semin Neurol. 1986;6:142-146.
Tamhankar MA, Biousse V, Ying GS, et al. Isolated third, fourth, and sixth cranial nerve palsies from
presumed microvascular versus other causes: a prospective study. Ophthalmology. 2013;120(11):
2264-2269.
Wilson-Pauwels L, Akesson EJ, Stewart PA. Cranial nerve VI: abducens nerve. In: Cranial Nerves: Anatomy and Clinical Comments. Philadelphia, PA: B.C. Decker; 1988:71-79.

0 comments:
Post a Comment
Note: Only a member of this blog may post a comment.