Median Nerve Mononeuropathy Case File
Eugene C. Toy, MD, Ericka Simpson, MD, Pedro Mancias, MD, Erin E. Furr-Stimming, MD
CASE 42
A 45-year-old female right-handed office assistant presents with a 5-month complaint of numbness and pain of her right index and middle fingers, which is worse with driving or typing on her keyboard at work. The symptoms often awaken her from sleep. She has also recently noticed difficulty fastening buttons using her right hand. Her medical history is only significant for a diagnosis with hypothyroidism 7 months previously. Her neurologic and physical examinations are significant for numbness to pinprick sensation along the right side of her palm, thumb, and index and middle fingers of her right hand. There is only mild weakness of thumb abduction. Symptoms are worsened with tapping on the ventral or palm side of her wrist. The rest of her examination, including muscle and sensory testing, are normal. Her deep tendon reflexes are normal throughout. There are no musculoskeletal or joint abnormalities observed.
▶ What is the most likely diagnosis?
▶ What is the next diagnostic step?
▶ What is the next step in therapy?
ANSWERS TO CASE 42:
Median Nerve Mononeuropathy
A 45-year-old right-handed office assistant with hypothyroidism presents with a 5-month complaint of numbness and pain of her right index and middle fingers, worsened with activity of the fingers. The symptoms often awaken the patient from sleep. There are both motor and sensory deficits of the median nerve distribution. There is a positive Tinel sign. The rest of her examination, including muscle and sensory testing, are normal. Her deep tendon reflexes are normal throughout.
- Most likely diagnosis: Right median nerve mononeuropathy at the wrist (carpal tunnel syndrome [CTS])
- Next diagnostic step: Electromyography (EMG) and nerve conduction studies (NCSs)
- Next step in therapy: Wrist splints, analgesics, rehabilitation, surgical evaluation
- Know the signs and symptoms of median mononeuropathy.
- Be familiar with the differential diagnosis of focal weakness and sensory deficits.
- Be familiar with the treatment and management of median nerve mononeuropathy.
Considerations
The patient presents with signs and symptoms of focal right hand numbness, pain, and weakness. Her examination reveals sensory deficit affecting the lateral aspect of the hand and fingers. Symptoms are worsened or reproduced with tapping or pressure on the anterior or palm side of her wrist. Her examination is otherwise normal. Her clinical history is also significant for working as an office assistant with associated worsening of symptoms with typing, in addition to driving and while sleeping. Based on this presentation, the site of lesion is likely located at the wrist. The distribution of her sensory and motor impairment to the lateral aspect (thumb side) of her palm and second to fourth digits of her hand fits the distribution of the median nerve, which is innervated by cervical roots 5 to 8 and thoracic root 1 originating from the spinal cord on the same side and coming through the lateral and medial cords of the brachial plexus. This presentation is consistent with a right median mononeuropathy at the wrist or CTS, although nerve root compression of these nerve roots at the level of the cervical spine or involvement of the plexus of nerves of the arm should be considered in the differential diagnosis.
APPROACH TO:
Carpal Tunnel Syndrome
DEFINITIONS
CARPAL TUNNEL: A narrow, rigid passageway of ligament and bones at the base of the hand through which the median nerve travels.
TINEL SIGN: Reproduction of numbness, tingling, or pain with tapping or pressing on the median nerve at the level of the patient’s wrist.
PHALEN SIGN: Test involves having the patient hold his or her forearms upright by pointing the fingers down and pressing the backs of the hands together. The presence of CTS is suggested if one or more symptoms, such as tingling or increasing numbness, is felt in the fingers within 1 minute.
CERVICAL RADICULOPATHY: Results from mechanical nerve root compression or intense inflammation of nerve root(s) (ie, radiculitis), resulting in an acute shooting pain and/or weakness in the distribution of that nerve root.
BRACHIAL PLEXOPATHY: Bundle of nerves that lies between the neck and the axilla with the distal portion lying behind the clavicle and the pectoral muscles. It is formed from the C5, C6, C7, C8, and T1 nerve roots and is best understood by dividing it into three parts: trunks, divisions, and cords.
CLINICAL APPROACH
Epidemiology and Clinical Features
CTS occurs when the median nerve, which runs from the forearm into the hand, becomes pressed or squeezed at the wrist. The median nerve controls sensations to the palm side of the thumb (I), index finger (II), middle finger (III), and lateral (thumb side) of the ring finger (IV) as well as impulses to some small muscles in the hand that allow the thumb to abduct and oppose (abductor pollicis brevis and opponens pollicis). The carpal tunnel is a narrow, rigid passageway of ligament and bones at the base of the hand, which houses the median nerve and flexor tendons. The cause of median nerve compression in the carpal tunnel can be related to repetitive use, which is hypothesized to result in compression of the nerve through frequent wrist flexion and extension.
Multiple factors can contribute to the development of median nerve compression, such as a congenitally small carpal tunnel, edema, inflammatory disorders, injury, anomalous muscle, a persistent median artery, neoplasm, or anything that would compress on the carpal tunnel or limit movement of the contents of the carpal tunnel. Systemic diseases can also be a part of the etiology of CTS, such as overactivity of the pituitary gland (eg, acromegaly), hypothyroidism, diabetes, rheumatoid arthritis, pregnancy, sarcoidosis, hereditary liability to pressure palsies, amyloidosis, multiple myeloma, leukemia, and aromatase inhibitors. There is little clinical data to prove whether repetitive and forceful movements of the hand and wrist during work or leisure activities can cause CTS. Repeated motions performed in the course of normal work or other daily activities can result in repetitive motion disorders such as bursitis and tendonitis. Writer’s cramp—a condition in which a lack of fine motor skill coordination and ache and pressure in the fingers, wrist, or forearm is brought on by repetitive activity—is not a symptom of CTS.
CTS is the most common entrapment neuropathy. Women are three times more likely than men to develop CTS, perhaps because the carpal tunnel itself can be smaller in women than in men. The dominant hand is usually affected first and produces the most severe pain. CTS usually occurs only in adults and is most frequent between 40 and 60 years. Only 10% of CTS patients are younger than 31 years. In the United States, the incidence is 1 to 3 cases per 1000 subjects per year; prevalence is approximately 50 cases per 1000 subjects in the general population. Incidence can increase as high as 150 cases per 1000 subjects per year, with prevalence rates greater than 500 cases per 1000 subjects in certain high-risk groups. Whites are probably at highest risk. The syndrome appears to be very rare in other non-white racial groups.
Compression of the median nerve in the carpal tunnel can result in pain, weakness, or numbness in the hand and wrist, radiating up the arm, with sparing of the more proximal muscles and sensory regions. The symptoms are gradual in onset and include burning, tingling, or itching numbness in the palm of the hand and the fingers, especially the thumb and the index and middle fingers. Often patients will complain of swelling in the hand or coldness, and on examination, the hand is not swollen or cold. This is due to altered sensation in the hand. The symptoms often first appear in one or both hands during the night, because many people sleep with flexed wrists. A person with CTS can wake up feeling the need to “shake out” the hand or wrist. As symptoms worsen, people might feel tingling during the day. Decreased strength may make it difficult to pick up small objects, fasten buttons, or perform other fine manual tasks involving thumb opposition. In chronic and/or untreated cases, the muscles at the base of the thumb can have signs of atrophy. It is important to compare muscle bulk between both hands. Not infrequently, patients report symptoms in the whole hand, but they often will say the fifth digit is spared after careful questioning. In rare cases, there are complaints of changes in sweating, which is due to loss of autonomic innervation (the median nerve carries most autonomic fibers to the whole hand).
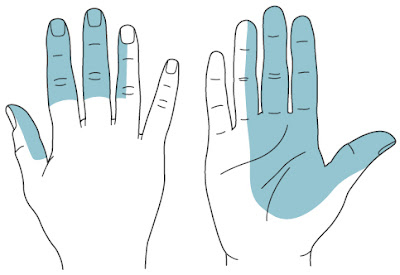
DIAGNOSIS
Early diagnosis and treatment are important to avoid permanent damage to the median nerve. A physical examination of the hands, arms, shoulders, and neck can help determine if the patient’s complaints are related to daily activities or to an underlying disorder and can rule out other painful conditions that mimic CTS. Carpal tunnel mimic syndromes include cervical radiculopathies or brachial plexopathies that can affect more than one nerve root or peripheral nerve. Cervical radiculopathy results from mechanical nerve root compression or intense inflammation of nerve root(s) (ie, radiculitis), resulting in an acute shooting pain in the distribution of that nerve root. The cervical region accounts for up to one- third of all radiculopathies encountered, with C7 being the most prevalent. However, the distribution of numbness, pain, or weakness will often follow the distribution of the nerve roots(s). As nerve roots contribute to more than one nerve, radiculopathies often affect muscles and dermatomal patterns of more than one peripheral nerve. This is often a clue to distinguish between a mononeuropathy and a radiculopathy. This likewise applies to conditions affecting the brachial plexus, which often involves more than one nerve. Although the median nerve is innervated by cervical roots C5 to C8 and thoracic root T1, these same roots also provide innervation to other peripheral nerves of the shoulder and arm. The median nerve provides motor and sensory innervation to the lateral, flexor compartment of the forearm and hand (Figure 42–1).
Clinically, the wrist is examined for tenderness, swelling, warmth, and discoloration. Each finger should be tested for sensation, and the muscles at the base of the hand should be examined for strength and signs of atrophy, with particular assessment of thumb opposition and abduction. Maneuvers should be performed to attempt to reproduce the symptoms, such as the Tinel test, in which the palmer aspect of the wrist is percussed and a positive test results in pain or tingling in the distribution of the median nerve or a shock sensation felt by the patient. The Phalen maneuver involves having the patient hold the forearms upright by pointing the fingers down and pressing the backs of the hands together. Alternatively, the hands can be extended with the palmer surfaces in opposition. This pose is held for 1 minute or until symptoms occur. The presence of CTS is suggested if one or more symptoms, such as tingling or increasing numbness, is felt in the fingers within 1 minute.
Confirmation of CTS can be obtained with electrodiagnostic tests, EMG/NCSs. In an NCS, electrodes are placed on the hand and wrist. Small electric shocks are applied, and the speed with which nerves transmit impulses is measured. In EMG, a fine needle is inserted into a muscle, and muscle activity or irritability can be recorded. The results of this test can determine the severity of damage to the median nerve. If CTS is very mild, these tests can be normal. Ultrasound imaging can also be performed to show impaired movement of the median nerve within the carpal tunnel or increased size indicating inflammation, and it is a useful complement to electrodiagnostic testing. MRI can show the anatomy of the wrist but to date has not been especially useful in diagnosing CTS. Blood tests can be performed to identify medical conditions associated with CTS. Routine laboratory tests such as thyroid hormone levels, complete blood counts, and blood sugar and proteins can reveal diabetes, hypothyroidism, arthritis, and fractures. X-ray tests of the wrist and hand might also be helpful to identify fractures.
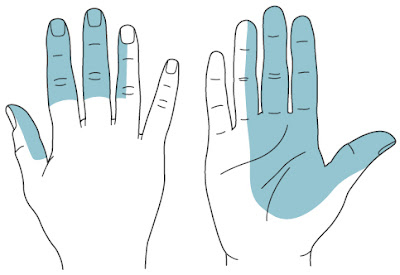
Figure 42–1. Sensory distribution for the median curve.
TREATMENT
Treatments for CTS should begin early after symptoms occur, and the least invasive treatments should be tried first. Underlying medical condition, such as diabetes or arthritis, should be treated while conservative treatment for CTS is initiated. Initial treatment generally involves resting the affected hand and wrist for at least 2 weeks, avoiding activities that can worsen symptoms, and immobilizing the wrist in a splint to avoid further damage from twisting or bending. The splint should be worn as much as possible during these 2 weeks, especially at night. If there is inflammation in the wrist, applying cool packs can help reduce swelling. Nonsteroidal anti-inflammatory drugs, such as ibuprofen and other nonprescription pain relievers, can ease symptoms that have been present for a short time or have been caused by strenuous activity. Orally administered diuretics can decrease swelling if edema is a contributing factor.
Corticosteroids (such as prednisone) or the drug lidocaine can be injected directly into the wrist or taken by mouth (in the case of prednisone) to relieve pressure on the median nerve and provide immediate, temporary relief to persons with mild or intermittent symptoms. Corticosteroid injections can also be used in patients with more severe symptoms who are unable to undergo surgery, such as pregnant women. Vitamin B6 (pyridoxine) supplements have been shown to ease the symptoms of CTS. Stretching and strengthening exercises, such as yoga, can be helpful in people whose symptoms have abated, but these should be limited during a flare. Ideally, a physical therapist or an occupational therapist should define a therapy and exercise regimen. Acupuncture and chiropractic care have benefited some patients, but their effectiveness remains unproved.
If these measures fail to relieve symptoms or if the symptoms progress and atrophy and weakness become evident, then surgery is the next option for treatment of CTS. Carpal tunnel release is one of the most common surgical procedures performed in the United States. Surgical treatment is indicated if there is CTS with significant atrophy, symptoms have persisted despite conservative treatment; there is persistent sensory impairment or intractable paresthesia/pain; there is improvement of symptoms after a corticosteroid injection with recurrence after the effect wears off; or there is a mechanical etiology (mass, fracture, etc). The surgery involves severing the band of tissue around the carpal tunnel (the flexor retinaculum) to reduce pressure on the median nerve. Surgery is done under local anesthesia and is an outpatient procedure. Many patients require surgery on both hands. Open release surgery is the traditional procedure used to correct CTS and consists of making an incision up to 2 inches in the wrist and then cutting the carpal ligament to enlarge the carpal tunnel. Endoscopic surgery may allow faster functional recovery and less postoperative discomfort than traditional open release surgery. Although symptoms may be relieved immediately after surgery, full recovery from carpal tunnel surgery can take months. Some patients can have infection, nerve damage, stiffness, and pain at the scar. Occasionally, the wrist loses strength because the carpal ligament is cut.
On NCS/EMG, if there are signs of axonal loss, initial surgical management should be considered to prevent any further permanent nerve damage. Overall, the complication rate is less than 1%. Surgery can be very successful, even in severe cases of CTS. Surgery is 90% effective and has a 60% success rate at 5 years. Patients should undergo physical therapy after surgery to restore wrist strength. Some patients may need to adjust job duties or even change jobs after recovery from surgery. Recurrence of CTS following surgical treatment is rare. The majority of patients recover completely. If CTS recurs soon after treatment or is not improved, then an evaluation for a more systemic neuropathy or etiology should be sought. At the workplace, ergonomic changes can be made to the work environment to minimize repetitive stress to the median nerve and allow the wrist to be in a neutral position. Conditioning and stretching exercises can be performed at work, frequent rest breaks may be indicated during specific tasks, wearing wrist splints may be necessary, and careful attention should be paid to posture and wrist position. However, research has not conclusively shown that these workplace changes prevent the occurrence of CTS.
COMPREHENSION QUESTIONS
Match the clinical descriptions (42.1-42.3) with the correct diagnosis (A-E). Choose an answer only once.
A. C6 radiculopathy
B. Brachial plexopathy
C. Focal myositis
D. Median mononeuropathy
E. Motor neuron disease
42.1 A 42-year-old man presents with a radiating pain from his neck to his elbow with numbness and tingling in the lateral ventral aspect of his right forearm and lateral palm. Examination reveals decreased sensation of the lateral anterior forearm as well as a decreased biceps reflex on the right.
42.2 A 53-year-old woman presents with numbness and pain in her hands, which often awaken her from sleep. She has noticed decreased ability to pick up small items, such as a penny or paper clip. Her examination reveals decreased sensation on the thenar surface of both hands, right greater than left. She also has decreased sensation of digits II and III of both hands. There is a small degree of muscle atrophy of the right thenar muscle.
42.3 A 65-year-old woman with a history of left breast cancer status postmastectomy and lymph node irradiation presents with painless weakness and numbness of her left shoulder and arm muscles and decreased ability to open or close her left hand. Examination reveals muscle atrophy and muscle twitches of the left hand intrinsic muscles, biceps, deltoids, and scapular muscles. The biceps and brachioradialis reflexes are absent.
ANSWERS
42.1 A. A C6 radiculopathy should be considered with a patient who presents with radiating pain in the presence of symptoms and signs that extends beyond one single nerve but is consistent with one or two nerve roots. This patient’s symptoms involve the elbow, forearm, lateral palm, and biceps reflex.
42.2 D. Median mononeuropathy. This patient has the classic presentation of CTS. She has bilateral pain, numbness, and weakness in distribution of median nerve.
42.3 B. Brachial plexopathy. This 65-year-old woman has muscle weakness, atrophy, and sensory deficit in distribution of more than one nerve (median, ulnar, radial, musculocutaneous), and more than one nerve root (C5-C7), which suggests brachial plexopathy. History of prior radiation is a risk factor for this brachial plexopathy.
CLINICAL PEARLS
|
▶ CTS is the most common nerve
entrapment disorder.
▶ Patients with CTS usually complain of
pain and numbness of the thumb and index and middle fingers.
▶ If pain is not a symptom, the
diagnosis of CTS should be questioned.
▶ If the symptoms are relieved by an
injection of corticosteroids, then the diagnosis of CTS and a positive
response to surgery is more likely.
▶ The main differential diagnosis for
CTS is C7 radiculopathy.
|
REFERENCES
Assmus H, Bischoff C. Carpal and cubital tunnel and other, rarer nerve compression syndromes. Dtsch Arztebl Int. 2015;112(1-2):14-26.
Atroshi I, Gummesson C, Johnsson R, Ornstein E, Ranstam J, Rosén I. Prevalence of carpal tunnel syndrome in a general population. JAMA. 1999;282(2):153-158.
Bland JD. Treatment of carpal tunnel syndrome. Muscle Nerve. 2007;36(2):167-171. Review.
National Institute of Neurological Disorders and Stroke. Carpal tunnel syndrome fact sheet. http://www.ninds.nih.gov/disorders/carpal_tunnel/detail_carpal_tunnel.htm. Accessed Nov 1, 2016.
Preston DC, Shapiro BE. Electromyography and Neuromuscular Disorders: Clinical–Electrophysiologic Correlations. 3rd ed. London, UK: Elsevier; 2013.
Spagnolo F, Sestak I, Howell A, Forbes JF, Cuzick J. Anastrozole-induced carpal tunnel syndrome: results from the International Breast Cancer Intervention Study II Prevention Trial. J Clin Oncol. 2016;34(2):139-143.
Wilder-Smith EP, Seet RC, Lim EC. Diagnosing carpal tunnel syndrome—clinical criteria and ancillary tests. Nat Clin Pract Neurol. 2006;2(7):366-374.

0 comments:
Post a Comment
Note: Only a member of this blog may post a comment.