Tuberculosis (Pulmonary), Cavitary Lung Lesions Case File
Eugene C. Toy, MD, Gabriel M. Aisenberg, MD
Case 44
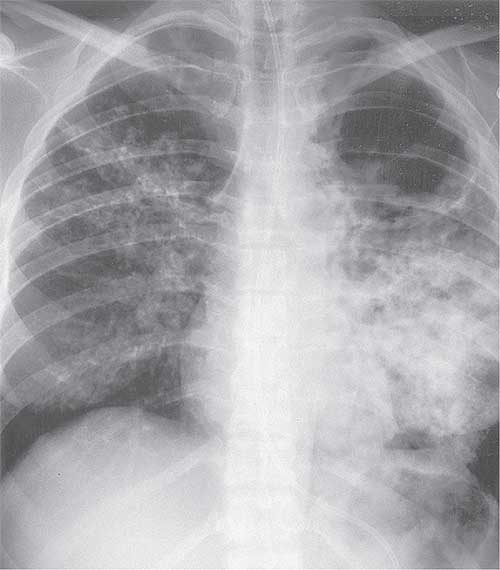
A 62-year-old man is brought to the clinic for a 3-month history of unintentional weight loss (12 lb). His appetite has diminished, but he reports no vomiting or diarrhea. He does report some depressive symptoms since the death of his wife a year ago, at which time he moved from Cambodia to the United States to live with his daughter. He denies a smoking history. He complains of a 3-month history of productive cough with greenish sputum. He has not felt feverish. He takes no medications regularly. On examination, his temperature is 100.4 °F and respiratory rate is 16 breaths per minute. His neck examination shows a normal thyroid gland and no cervical or supraclavicular lymphadenopathy. His chest has scattered crackles in the left midlung fields and a faint expiratory wheeze on the right. His heart rhythm is regular with no gallops or murmurs. His abdominal examination is benign, his rectal examination shows no masses, and his stool is negative for occult blood. His chest x-ray is shown in Figure 44–1.
▶ What is the most likely diagnosis?
▶ What is your next step?
Figure 44–1. Chest x-ray. (Reproduced with permission, from Fishman AP. Fishman’s Pulmonary Diseases and Disorders. 3rd ed. 1998. Copyright © McGraw Hill LLC. All rights reserved.)
ANSWERS TO CASE 44:
Tuberculosis (Pulmonary), Cavitary Lung Lesions
Summary: A 62-year-old man from Cambodia presents with
- A 12-lb unintentional weight loss over 3 months
- Diminished appetite
- A low-grade fever and productive cough
- A chest x-ray with right upper lobe reticulonodular pattern and a left lung cavitary lesion
Most likely diagnosis: Pulmonary tuberculosis (TB).
Next step: Serial sputum samples for identification of the organism and for culture and sensitivities to guide antimicrobial therapy.
- Recognize the natural history, clinical manifestations, and radiographic findings of primary, secondary, and latent TB infection. (EPA 1, 3)
- Understand the methods of diagnosis of TB. (EPA 1, 3)
- Describe treatment strategies for TB. (EPA 4)
- List the common extrapulmonary sites of TB infection, including the pleura, lymph nodes, meninges, genitourinary tract, skeletal system, adrenal glands, and miliary TB. (EPA 12)
Considerations
This elderly Asian man has symptoms suggestive of TB, including low-grade fever, weight loss, and productive cough. A chest radiograph is essential to establish the diagnosis. His chest x-ray shows findings consistent with TB, but many other diseases may cause cavitary lung lesions, including other infections and malignancies. If the sputum samples do not reveal acid-fast organisms, then further testing, such as bronchoscopy, may be needed.
LATENT TB: Asymptomatic infection with Mycobacterium tuberculosis.
PRIMARY TB: Development of clinical illness immediately after infection with M. tuberculosis.
REACTIVATION TB: Clinical illness that occurs when latent TB becomes active and infectious after a period of dormancy. The dormant period can last years after the initial infection.
CLINICAL APPROACH
Pathophysiology
Pulmonary TB. TB is a bacterial infection caused by the acid-fast bacillus (AFB) M. tuberculosis, which is usually transmitted through airborne spread of droplets from infected patients with pulmonary TB. Most cases occur in developing countries, but a resurgence of cases in the United States occurred during the mid-1980s as a consequence of various factors, including human immunodeficiency virus (HIV) infection. Untreated disease can have a 1-year mortality rate of 33% and a 5-year mortality rate as high as 50%.
Often seen in children, primary pulmonary TB usually affects the middle and lower lobes. Lesions form in the periphery with hilar and paratracheal lymphadenopathy. Granulomatous lesions are caused by the inflammatory response of lymphocytes and macrophages with cytokines such as tumor necrosis factor alpha (TNF alpha). The center of the lesion may become necrotic (caseous necrosis) and liquefied, forming a cavity. Healed lesions are called Ghon lesions. Most patients exposed to M. tuberculosis do not manifest clinical symptoms, but they may have a latent infection. Years later, TB may reactivate and become symptomatic. Reactivation TB usually involves the apical and posterior segments of the upper lobes or the superior segments of the lower lobes of the lungs. The course may be rapid (weeks to months), chronic and slowly progressive (“consumption”), or spontaneously remit.
Signs and symptoms are nonspecific and subacute, including fever, night sweats, malaise, weight loss, and anorexia. The cough usually is productive of purulent sputum and sometimes is streaked with blood. A Rasmussen aneurysm sometimes develops in proximity to a cavitary lesion as the inflammatory reaction causes thinning of the wall of an adjacent bronchial artery. Rupture of the aneurysm can lead to massive hemoptysis. Physical findings are nonspecific and can include fever, wasting, crackles and rhonchi, pallor, or finger clubbing. Possible laboratory abnormalities are leukocytosis, anemia, and hyponatremia secondary to the syndrome of inappropriate secretion of antidiuretic hormone.
Extrapulmonary TB. The sites of extrapulmonary spread of TB, in order of decreasing frequency of occurrence, are the lymph nodes, pleura, genitourinary
tract, bones and joints, meninges, and peritoneum. TB lymphadenitis is common in HIV-infected patients, children, and nonwhite women, and it generally manifests as painless adenopathy. Pleural disease can have an exudative effusion but may require pleural biopsy for diagnosis. TB meningitis is usually diagnosed by finding cerebrospinal fluid with high protein, lymphocyte predominance (or neutrophils in early infection), and low glucose level. Adjunctive glucocorticoids may improve the treatment response in TB meningitis. Genitourinary TB can be asymptomatic or have local symptoms such as dysuria, hematuria, and urinary frequency. It is characterized by the finding of leukocytes in the urine but negative bacterial cultures—termed “sterile pyuria.” Skeletal TB affects weight-bearing joints, whereas Pott disease involves the spine. Miliary TB refers to hematogenously disseminated TB and describes the radiographic or pathologic finding of 1- to 2-mm granulomas that resemble millet seeds (hence the name). Adrenal involvement is common in miliary TB and may cause adrenal insufficiency.
Diagnosis. The diagnosis of TB is made by combining the history and clinical picture with AFB stains or culture of a specimen (smear or tissue biopsy). When pulmonary TB is suspected, three sputum samples should be obtained while the patient is on isolation if hospitalized. At least one of these should be collected in the early morning. Biopsy material should not be put in formaldehyde. Culture results may take from 4 to 8 weeks on ordinary solid media or 2 to 3 weeks on liquid media.
Nucleic acid amplification testing (NAAT) should also be performed on patients with signs of active pulmonary TB disease. This is done through a sputum sample as well, typically on the first respiratory specimen sent for AFB stains. Although NAAT can help confirm the diagnosis of TB and may prompt earlier initiation of treatment, it should not be used as a substitution for AFB testing. Confirmed TB cases should be reported to the local public health department.
Purified protein derivative (PPD), or tuberculin, skin testing is useful for screening for latent TB infection but has a limited role in diagnosing active infection because of frequent false-negative results in this setting. A positive PPD is defined by induration of at least 5 mm after 48 to 72 hours, although this can vary based on the risk group (Table 44–1).
Interferon-gamma release assays (IGRAs) are new diagnostic tools for latent TB. They are in vitro blood tests of cell-mediated immune response to M. tuberculosis and measure T-cell release of interferon-gamma (IFN-gamma) following stimulation by TB antigens. The Centers for Disease Control and Prevention (CDC) recommends that such tests can be used in place of tuberculin skin testing. IGRAs are preferred for patients with a history of bacille Calmette-Guérin (BCG) vaccination (it is not affected by BCG). It requires only one visit (PPD requires a second visit to read the result 2 days after its intradermal administration). The most commonly used IGRAs are the QuantiFERON™-TB Gold assay and the T-SPOT™ TB assay.
Treatment
The probable resistance pattern of the TB organism, based on the country of origin, may help to guide treatment. For individuals from areas with low drug resistance, therapy generally starts with a 2-month course of four-drug treatment with isoniazid (INH), rifampin, pyrazinamide, and ethambutol, followed by 4 months of INH and rifampin. Multiple drugs are used to avoid development of resistance. Directly observed treatment (watching patients take the medication) should be instituted in all patients in this phase to ensure compliance. Pyridoxine is frequently added to the regimen to prevent peripheral neuropathy caused by INH.
Reproduced with permission,from Longo DL, Fauci AS, Kasper DL, et al, eds. Harrison’s Principles of Internal Medicine. 18th ed. 2012. Copyright © McGraw Hill LLC. All rights reserved.
Drug resistance or intolerable side effects may require alternate therapy. Patients should be monitored for hepatitis, hyperuricemia, and cytopenias—especially thrombocytopenia—as these can indicate drug toxicity. The World Health Organization defines treatment failure as a positive smear or culture after 5 months of therapy. Latent TB infection is usually treated with INH for 9 months or rifampin for 4 months, with the goal of preventing reactivation TB later in life. Extrapulmonary TB sometimes requires longer therapy, which varies depending on the affected organ.
CASE CORRELATION
- See also Case 15 (Chronic Obstructive Pulmonary Disease), Case 16 (Chronic Cough/Asthma), Case 18 (Hemoptysis/Lung Cancer), and Case 19 (Community-Acquired Pneumonia).
COMPREHENSION QUESTIONS
44.1 A 42-year-old woman from Pakistan is being treated with infliximab, a TNF alpha blocker, for rheumatoid arthritis. After 6 months of therapy, she develops persistent fever, weight loss, and night sweats, and TB is suspected. Which of the following is the most likely location of the TB?
A. Middle and lower lung zones
B. Pleural space
C. Apical segment of the upper lung lobes
D. Cervical or supraclavicular lymph nodes
44.2 A 24-year-old man is being seen in the office for his monthly follow-up for treatment with INH, rifampin, and pyrazinamide for active pulmonary TB. He has been taking his medications for 3 months. While his cough and fever are now resolved, he states that he is having numbness and tingling of both feet but no back pain. He denies taking other medications. Which of the following is the most appropriate next step?
A. Perform a computed tomography (CT) scan of the lumbar spine.
B. Initiate pyridoxine.
C. Continue the TB agents and monitor for further neurologic problems.
D. Initiate a workup for TB adenopathy compression on the femoral nerve.
44.3 A 25-year-old woman is seen in the clinic because her father, who recently emigrated from South America, was diagnosed with and has been treated for TB. She denies a cough, and her chest radiograph is normal. A PPD test shows 10 mm of induration. Her only medication is an oral contraceptive. Which of the following is the best next step?
A. Isoniazid
B. Combination therapy, including INH, rifampin, and pyrazinamide
C. Observation
D. Induce three sputum samples
44.4 A 56-year-old woman is being seen at a pulmonary clinic for a chronic cough and weight loss. She is diagnosed with pulmonary TB. She denies having medical problems. The planned therapy includes INH and rifampin. Which of the following tests are the most important to follow for a patient receiving these agents for her TB treatment?
A. Renal function tests
B. Liver function tests
C. Slit-lamp examinations
D. Amylase and lipase tests
ANSWERS
44.1 C. Reactivation TB (in this case, likely triggered by infliximab) usually involves the apical aspects of the lungs. Primary pulmonary TB infection most often affects the middle and lower lobes (answer A). Lymphadenitis (answer D) and pleural disease (answer B) are the most common extrapulmonary TB infections, but they are less common than pulmonary TB.
44.2 B. Pyridoxine (vitamin B6) is important for preventing the peripheral neuropathy that can complicate INH therapy. Assuming that his neurologic examination is normal other than some minimal decreased sensation, initiation of pyridoxine and careful monitoring is the best course of action. If the physical examination shows weakness, abnormal deep tendon reflexes, or dermatomal distribution, then imaging of the lumbar spine such as CT scan (answer A) would be indicated. If the numbness were caused by Pott disease, he would be expected to have back pain and other neurologic findings, such as lower extremity weakness. Continuing therapy without pyridoxime is inappropriate (answer C), and vitamin B6 should have been started at the onset of his therapy. Workup for femoral nerve impingement (answer D) is not indicated unless the physical examination points to a pure femoral nerve palsy.
44.3 A. Because this woman is a household contact of a patient with active TB, she is in the highest risk group. Her skin test would be considered positive with 5-mm induration. Therefore, observation (answer C) would be inappropriate, and inducing three sputum samples (answer D) would not be required. She has latent TB infection and should be offered treatment to prevent reactivation TB later in life. INH is the treatment of choice for exposure prophylaxis. Rifampin offers a safe alternative for a shorter duration. Triple therapy (answer B) is indicated for an active TB infection, but not for a contact asymptomatic situation.
44.4 B. Drug-induced liver injury is a complication of treatment with INH, pyrazinamide, and rifampin; therefore, liver enzyme levels are the most important parameters to monitor. Baseline liver tests are obtained in all patients, and monthly monitoring of hepatic enzymes is recommended for patients at increased risk of liver toxicity. Alcohol use, prior liver disease, pregnancy, and the first 3 months postpartum are risk factors for liver injury. Renal (answer A) and pancreatic (answer D) functions are not as much of a concern with drugs used to treat TB. Slit-lamp examinations assess the anterior chamber of the eye (answer C) and are indicated for medications such as amiodarone, which can cause corneal deposits; the TB drug that can lead to blindness is ethambutol, but this would be an optic neuritis and not detected on slit-lamp examination.
CLINICAL PEARLS
▶ Reactivation pulmonary TB most commonly presents radiographically with opacities in the apical and posterior segments of the upper lobes.
▶ Tuberculin skin testing is not a diagnostic test but is a useful screening test for potential contacts of infected persons; the response cutoff for a positive test depends on the patient’s level of risk. IGRAs such as QuantiFERON®-TB Gold are also useful to diagnose latent TB.
▶ Patients with a positive tuberculin skin test and no clinical or radiographic evidence of active disease are said to have latent TB infection; they can be treated with INH or rifampin to reduce their lifetime risk of developing reactivation TB.
▶ Individuals with active TB should be initiated on multidrug therapy, such as INH, rifampin, pyrazinamide, and ethambutol.
▶ Pyridoxine (vitamin B6) is usually added to antituberculosis medications to prevent peripheral neuropathy.
REFERENCES
Blumberg HM, Burman WJ, Chaisson RE, et al. American Thoracic Society/Centers for Disease Control and Prevention/Infectious Diseases Society of America: treatment of tuberculosis. Am J Respir Crit Care Med. 2003;167:603-662.
Campbell IA, Bah-Sow O. Pulmonary tuberculosis: diagnosis and treatment. BMJ. 2006;332:1194-1197.
Jasmer RM, Nahid P, Hopewell PC. Latent tuberculosis infection. N Engl J Med. 2002;347:1860-1866.
Mazurek GH, Jereb J. Updated guidelines for using interferon gamma release assays to detect Mycobacterium tuberculosis infection—United States, 2010. MMWR Recomm Rep. 2010;59(RR-5):1.
Raviglione MC, O’Brian R. Tuberculosis. In: Jameson JL, Fauci AS, Kasper DL, et al, eds. Harrison’s Principles of Internal Medicine. 20th ed. New York, NY: McGraw Hill; 2018:1340-1359.
Zumla A, Raviglione M, Hafner R, et al. Tuberculosis. N Engl J Med. 2013;368:745-755.


0 comments:
Post a Comment
Note: Only a member of this blog may post a comment.