Painless Jaundice, Pancreatic Cancer Case File
Eugene C. Toy, MD, Gabriel M. Aisenberg, MD
Case 27
A 57-year-old man comes to the clinic complaining of malaise for several weeks. He says that he has not been feeling well for some time, with fatigue, depressed mood, loss of appetite, and a 20-lb unintentional weight loss. In addition, he has been bothered by generalized itching of his skin and has tried moisturizing lotions and creams without improvement. He denies fevers, abdominal pain, nausea, vomiting, or diarrhea. He does think his stools have been lighter in color recently. He has also noticed his urine is darker. He has no other medical history and takes no medications except for a multivitamin. He drinks alcohol occasionally and smokes cigars.
On examination, he is afebrile, with heart rate of 68 beats per minute (bpm) and blood pressure of 128/74 mm Hg. He has a flat affect and a somewhat disheveled appearance. He has noticeable icterus of his sclera and skin. His chest is clear, and his heart rhythm is regular without murmurs. His abdomen is soft and nontender with active bowel sounds, a liver span of 10 cm, and no splenomegaly or masses. His skin has a few excoriations on his arms and back, but no rashes or telangiectasias are present.
Blood is obtained for laboratory analysis; the results are available the next day. His serum albumin is 3.1 g/dL, alkaline phosphatase 588 IU/L, total bilirubin 8.5 mg/dL, direct bilirubin 6 mg/dL, alanine aminotransferase (ALT) 175 IU/L, and aspartate aminotransferase (AST) 140 IU/L. His hemoglobin level is 13.5 g/dL. Prothrombin time (PT) is 15 seconds, international normalized ratio (INR) is 1.2, and partial thromboplastin time is 32 seconds.
▶ What is the most likely diagnosis?
▶ What is the next diagnostic step?
▶ What risk factors are associated with the most likely diagnosis?
ANSWERS TO CASE 27:
Painless Jaundice, Pancreatic Cancer
Summary: A 57-year-old man presents with
- Pruritus and weight loss
- Light-colored stools and dark urine
- Painless jaundice
- Elevated alkaline phosphatase level and conjugated hyperbilirubinemia
Most likely diagnosis: Biliary obstruction, most likely caused by malignancy.
Next diagnostic step: Imaging procedure of his biliary system, initially ultrasonography followed by computed tomographic (CT) scan.
Risk factors for pancreatic cancer: Smoking, alcohol use, obesity, age, and diabetes.
ANALYSIS
Objectives
- Describe the causes and evaluation of a patient with unconjugated hyperbilirubinemia. (EPA 1, 2, 3)
- Distinguish between hepatocellular disease and biliary obstruction. (EPA 3)
- Evaluate patients with cholestasis. (EPA 1, 3)
- List the treatment and complications of biliary obstruction. (EPA 4, 10)
Considerations
In patients with jaundice, one must try to distinguish between hepatocellular and biliary disease. In a patient with painless biliary obstruction, one should be suspicious of malignancy or strictures. The findings in this case, such as generalized pruritis and icterus, point toward cholestasis. The light-colored or acholic stools suggest the cholestasis is most likely due to biliary obstruction since bile is what causes stool to have its darker color. The absence of abdominal pain makes gallstone disease less likely, and in fact, nontender jaundice is suspicious for pancreatic cancer.
APPROACH TO:
Painless Jaundice
DEFINITIONS
CHOLESTASIS: Deficient bile flow that can result from intrahepatic disease or extrahepatic obstruction.
CONJUGATED BILIRUBIN (DIRECT-REACTING BILIRUBIN): Bilirubin that has entered the liver and has been enzymatically bound to glucuronic acid, forming the water-soluble bilirubin monoglucuronide or diglucuronide.
JAUNDICE OR ICTERUS: Yellowing of the skin or whites of the eyes, indicating hyperbilirubinemia.
UNCONJUGATED BILIRUBIN (INDIRECT-REACTING BILIRUBIN):
Bilirubin that has not been enzymatically bound to glucuronic acid by the liver and is in the serum reversibly and noncovalently bound to albumin.
CLINICAL APPROACH
Pathophysiology
Jaundice, or icterus, is the visible manifestation of hyperbilirubinemia and usually can be noticed by physical examination when the serum bilirubin level exceeds 2.0 to 2.5 mg/dL. Traditional instruction regarding the jaundiced patient divides the mechanism of hyperbilirubinemia into prehepatic (excessive production of bilirubin), intrahepatic, or extrahepatic (as in biliary obstruction). For most patients with jaundice, the focus should be on hepatic or biliary diseases that cause conjugated (direct) hyperbilirubinemia because they represent the most clinically important causes of jaundice.
The term unconjugated (indirect) hyperbilirubinemia is used when the conjugated (or direct-reacting fraction) does not exceed 15% of the total bilirubin. In adults, it is almost always caused by hemolysis or Gilbert syndrome. In these conditions, the serum bilirubin level almost always is less than 5 mg/dL, and there are usually no other clinical signs of liver disease. In addition, there should be no bilirubinuria (only conjugated bilirubin can be filtered and renally excreted). Hemolysis usually is clinically apparent, as in sickle cell disease or autoimmune hemolytic anemia. Gilbert syndrome is a benign condition caused by a deficiency of hepatic enzymatic conjugation of bilirubin, which results in intermittent unconjugated hyperbilirubinemia. Total bilirubin is usually less than 4 g/dL and is often precipitated by events such as stress, fasting, and febrile illnesses. It is not associated with liver dysfunction and requires no therapy.
Conjugated (direct) hyperbilirubinemia almost always reflects either hepatocellular disease or biliary obstruction. These two conditions can be differentiated by the pattern of elevation of the liver enzymes. Elevation of serum AST and ALT levels is characteristic of hepatocellular disease as a result of the inflammation/destruction of the hepatocytes and the release of these enzymes into the blood.
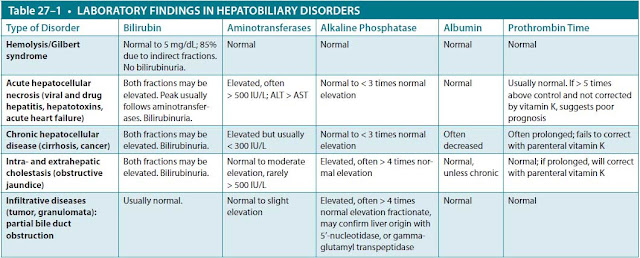
The serum alkaline phosphatase level is elevated in cholestatic disease as a consequence of inflammation, destruction, or obstruction of the intrahepatic or extrahepatic bile ducts with relative sparing of the hepatocytes. The serum AST and ALT levels may be mildly elevated in cholestasis but usually not to the levels seen in primary acute hepatocellular disease. Other tests, such as serum albumin or PT, generally reflect the capacity of hepatocytes to synthesize proteins such as clotting factors. When they are abnormal, they most often reflect hepatocellular disease. Table 27–1 summarizes the liver test patterns seen in various categories of hepatobiliary disorders.
Differential Diagnosis. The patient discussed in this case has a pattern consistent with cholestasis, and the first diagnostic test in a patient with cholestasis usually is an ultrasound. It is noninvasive and is very sensitive for detecting stones in the gallbladder as well as intrahepatic or extrahepatic biliary ductal dilation. The most common cause of biliary obstruction in the United States is gallstones, which may become lodged in the common bile duct. Obstructing stones causing jaundice usually are associated with epigastric or right upper quadrant colicky pain. Extrahepatic dilation without evidence of stones warrants further study with CT, magnetic resonance cholangiopancreatography, or endoscopic retrograde cholangiopancreatography (ERCP). These imaging techniques may detect occult stones, strictures, or malignancies that include cholangiocarcinoma, pancreatic cancer, and ampullary cancer (ampulla of Vater).
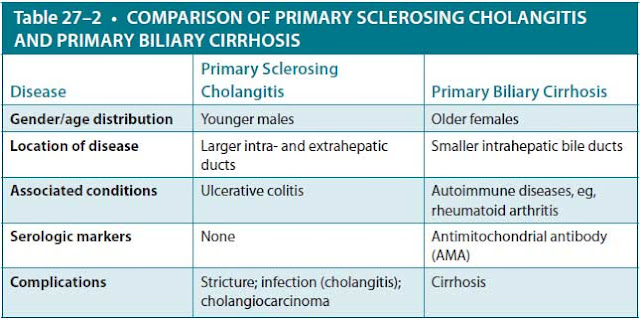
Other possible causes of obstruction include strictures, which can result from prior biliary surgery, prior inflammatory conditions such as pancreatitis (rarely), inflammatory diseases of the biliary tree, and infection in the setting of acquired immunodeficiency syndrome (AIDS). Two important primary biliary conditions are primary sclerosing cholangitis and primary biliary cirrhosis. Table 27–2 compares features of these two entities.
The complications of biliary obstruction include development of acute cholangitis as a result of ascending infection, or secondary hepatic cirrhosis if the obstruction is chronic or recurrent. The patient in this case scenario has painless jaundice, liver enzymes consistent with a cholestatic process, and light-colored stools, suggesting obstruction of bile flow into the intestine. Because he has no history of abdominal or biliary surgery that might have caused a stricture, malignancy is the most likely cause of his biliary obstruction. The most common malignancy with this clinical presentation is pancreatic cancer. The patient should undergo an imaging procedure of his abdomen, including a right upper quadrant ultrasound to evaluate the biliary tree, as well as a CT scan or magnetic resonance imaging (MRI) to visualize the pancreas. Endoscopic ultrasound with fine-needle aspiration of the pancreas is highly accurate in establishing a tissue diagnosis.
Treatment
Pancreatic cancer is the fifth leading cause of cancer death in the United States. Peak incidence is in the seventh decade of life, with two-thirds of cases occurring in persons older than 65 years. The median survival is 9 months, with a dismal overall 5-year survival rate of 3%. Clinically apparent metastatic disease is found in 80% of patients at the time of diagnosis. For patients without obvious metastases, the best
Reproduced with permission, form Braunwald E, Fauci AS, Kasper DL, et al., eds. Harrison’s Principles of Internal Medicine, 17th ed. 2008. Copyright © McGraw Hill LLc. All righs reserved.
hope for cure is surgical resection by pancreaticoduodenectomy (Whipple procedure), which in experienced hands has a perioperative mortality rate of less than 5%. Even when the cancer is resectable, there is a high rate of recurrence. As such, many treatment programs include neoadjuvant chemotherapy. Palliative measures may include common bile duct stenting to relieve biliary obstruction. Several serum markers for pancreatic cancer have been evaluated, the most useful of which is CA 19-9. This marker has prognostic value and is also used as an indicator of response to treatment and/or disease progression.
Unfortunately, there is no cure for primary biliary cirrhosis, but ursodeoxycholic acid, steroids, and immunosuppressive agents can slow the progression of the disease; ultimately, liver transplantation is the only option for end-stage disease.
CASE CORRELATION
- See also Case 24 (Liver Cirrhosis, Probably Alcoholic) and Case 26 (Acute Hepatitis).
COMPREHENSION QUESTIONS
For Questions 27.1 to 27.4, choose the one diagnosis (A-F) that best matches with the most likely clinical situation.
A. Hemolysis
B. Alcoholic hepatitis
C. Gilbert disease
D. Pancreatic cancer
E. Gallstones
F. Primary sclerosing cholangitis
27.1 A 38-year-old man with an alcohol history of 12 beers per day presents with jaundice, ascites, and dark urine. His laboratory results are AST 350 U/mL, ALT 150 U/mL, alkaline phosphatase 120 U/mL, total bilirubin 25 mg/dL, direct bilirubin 18 mg/dL, and albumin 2.1 g/dL.
27.2 A 40-year-old moderately obese woman presents with abdominal pain after eating and mild conjunctival icterus. Her laboratory results are
AST 200 U/L, ALT 150 U/L, alkaline phosphatase 355 U/L, total bilirubin 3.5 mg/dL, direct bilirubin 1.8 mg/dL, and albumin 3.5 g/dL.
27.3 A 25-year-old man presents with 3 days of conjunctival icterus but has been otherwise feeling well. His laboratory results are AST 45 U/L, ALT 48 U/L, alkaline phosphatase 100 U/L, total bilirubin 3.2 mg/dL, direct bilirubin 0.2 mg/dL, and albumin 3.5 g/dL. Complete blood cell count and lactate dehydrogenase are normal.
27.4 A 32-year-old man with a 5-year history of episodic bloody diarrhea and abdominal cramping pain presents with conjunctival icterus and fever. His laboratory results are AST 100 U/L, ALT 125 U/L, alkaline phosphatase 550 U/L, total bilirubin 5.5 mg/dL, direct bilirubin 3.0 mg/dL, and albumin 2.9 g/dL.
ANSWERS
27.1 B. The patient’s laboratory results show a conjugated hyperbilirubinemia with evidence of hepatocellular disease (hypoalbuminemia, ascites). The AST and ALT levels show the 2:1 ratio consistent with alcohol-related liver disease.
27.2 E. The patient’s laboratory results show a conjugated hyperbilirubinemia consistent with an obstructive pattern. She has the risk factors for gallstones (female, obese, middle age) and has symptoms of postprandial abdominal pain.
27.3 C. The patient’s laboratory results show an unconjugated hyperbilirubinemia without other abnormality. He is otherwise healthy and without symptoms of systemic disease or hemolytic anemia; this is suggestive of Gilbert disease. No treatment is necessary.
27.4 F. The patient’s laboratory results show a conjugated hyperbilirubinemia with an obstructive pattern. The history is consistent with inflammatory bowel disease, which is associated with primary sclerosing cholangitis. The initial evaluation should include ultrasonography to rule out gallstones; if negative, ERCP could confirm the diagnosis by demonstrating multiple strictures of the extrahepatic bile ducts. Treatment options include stenting of the larger bile duct strictures and immunosuppression to slow the progression of the disease.
CLINICAL PEARLS
▶ Unconjugated (indirect) hyperbilirubinemia usually is caused by hemoly-sis or Gilbert syndrome.
▶ Conjugated (direct) hyperbilirubinemia is commonly caused by hepato-cellular disease, with elevated AST and ALT levels, or biliary obstruction, with elevated alkaline phosphatase level.
▶ An imaging procedure such as ultrasonography is the initial study of choice in a patient with cholestasis to evaluate for intrahepatic or extra-hepatic biliary obstruction.
▶ The most common causes of biliary obstruction are gallstones, which are painful if obstructing, and strictures or neoplasms, which may be painless.
▶ Pancreatic cancer is initially diagnosed and staged by CT; the best hope for cure is resection by a pancreaticoduodenectomy (Whipple procedure).
REFERENCES
Brugge WR, Dam JV. Medical progress: pancreatic and biliary endoscopy. N Engl J Med. 1999;341:1808-1916.
Mohammed S, Van Buren G 2nd, Fisher WE. Pancreatic cancer: advances in treatment. World J Gastroenterol. 2014;20(28):9354-9360.
Pratt DS. Evaluation of liver function. In: Jameson J, Fauci AS, Kasper DL, Hauser SL, Longo DL, Loscalzo J, eds. Harrison’s Principles of Internal Medicine. 20th ed. New York, NY: McGraw Hill; 2018.
Wolkoff AW. The hyperbilirubinemias. In: Jameson J, Fauci AS, Kasper DL, Hauser SL, Longo DL, Loscalzo J, eds. Harrison’s Principles of Internal Medicine. 20th ed. New York, NY: McGraw Hill; 2018.

0 comments:
Post a Comment
Note: Only a member of this blog may post a comment.