Acute Hepatitis Case File
Eugene C. Toy, MD, Gabriel M. Aisenberg, MD
Case 26
A 28-year-old man comes to your clinic complaining of a 5-day history of nausea, vomiting, diffuse abdominal pain, fever, and muscle aches. He has lost his appetite, but he is able to tolerate liquids and has no diarrhea. He has no significant medical or family history, and he has not traveled outside the United States. He admits to having 12 different lifetime sexual partners with inconsistent barrier protection use. He denies illicit drug use and reports drinking alcohol occasionally, but not since this illness began. He takes no medications or supplements. However, he has taken 30 tablets of acetaminophen per day over the past 2 days for fever and body aches. On examination, his temperature is 100.8 °F, heart rate is 98 beats per minute (bpm), and blood pressure is 120/74 mm Hg. He is alert and oriented but appears uncomfortable. Jaundice is noted. His chest is clear to auscultation, and his heart rhythm is regular without murmurs. His liver size is estimated to be 12 cm upon percussion and is noted to be smooth but slightly tender to palpation. He has no abdominal distention or peripheral edema. Laboratory values are significant for a normal complete blood count, creatinine 1.1 mg/dL, alanine aminotransferase (ALT) 3440 IU/L, aspartate aminotransferase (AST) 2705 IU/L, total bilirubin 24.5 mg/dL, direct bilirubin 18.2 mg/dL, alkaline phosphatase 349 IU/L, serum albumin 3.0 g/dL, and prothrombin time 14 seconds.
▶ What is the most likely diagnosis?
▶ What is the most important immediate diagnostic test?
▶ What is an important management consideration for this patient?
ANSWERS TO CASE 26:
Acute Hepatitis
Summary: A 28-year-old man presents with
- No past medical history
- Five days of nausea, vomiting, diffuse abdominal pain, fever, and myalgias
- Twelve different lifetime sexual partners
- Recent history of taking large amounts of acetaminophen
- Icteric appearance with a low-grade fever and tender hepatomegaly
- Laboratory results consistent with severe hepatocellular injury
Most likely diagnosis: Acute hepatitis, either viral infection or toxic injury, possibly exacerbated by acetaminophen use due to the patient’s young age, sexual history, lack of medication/supplement use, and pattern of liver study results.
Most important immediate diagnostic test: Acetaminophen level, as acetaminophen toxicity may greatly exacerbate liver injury but is treatable.
Important management consideration: If fulminant liver failure is suspected, the patient should be transferred to a liver transplant center to be evaluated, as fulminant liver failure may be rapidly fatal. Evaluate for encephalopathy in conjunction with hepatic synthetic dysfunction.
- Understand the use of viral serologic studies for diagnosing hepatitis A, B, and C infections. (EPA 3)
- Recognize the prognosis for acute viral hepatitis and recognize fulminant hepatic failure. (EPA 1, 12)
- List measures to prevent hepatitis A and B infections. (EPA 12)
- Understand the use of the acetaminophen nomogram and the treatment of acetaminophen hepatotoxicity. (EPA 3, 4)
Considerations
This patient has an acute onset of hepatic injury and systemic symptoms that pre-date his acetaminophen use. The markedly elevated hepatic transaminases and bilirubin levels are consistent with viral hepatitis or toxic injury. This patient denied intravenous drug use, which would be a risk factor for hepatitis B and C infections. However, his sexual history does place him at higher risk for these infections. The degree and pattern of transaminase ALT and AST elevation provide clues to help differentiate possible etiologies. Transaminase levels more than 1000 IU/L are seen in conditions that produce extensive hepatic necrosis, such as toxic injury, viral hepatitis, and ischemia (“shock liver”). Meanwhile, patients with alcoholic hepatitis almost always have levels less than 500 IU/L and often have an AST/ALT ratio of 2:1. In this case, it is important to consider the possibility of acetaminophen toxicity, both because the condition can produce fatal liver failure and because an effective antidote is available. By obtaining a serum acetaminophen level and knowing the time of his last ingestion, the provider can plot the data on a nomogram (Figure 26–1) to help predict acetaminophen-related liver damage and the possible need for N-acetylcysteine (NAC), which is the antidote.

Figure 26–1. Acetaminophen nomogram. (Reproduced with permission, from Braunwald E, Fauci AS, Kasper DL, et al., eds. Harrison’s Principles of Internal Medicine, 15th ed. 2001. Copyright © McGraw Hill LLC. All rights reserved.)
APPROACH TO:
Viral and Acetaminophen Hepatitis
DEFINITIONS
ACUTE HEPATITIS: Inflammation of the liver that may be caused by infection, ischemia, autoimmune state, or toxic exposure for a duration of less than 26 weeks. At least six viruses that cause hepatitis have been identified, referred to as hepatitis A, B, C, D, E, and G. Hepatitis A, C, D, E, and G are RNA viruses, while hepatitis B is a DNA virus.
CHRONIC HEPATITIS: A syndrome that is defined clinically by evidence of liver disease with inflammation and necrosis for at least 26 weeks, most commonly with hepatitis B, C, and D infections.
CIRRHOSIS: Diffuse damage to hepatocytes, which show evidence of chronic inflammation with fibrosis and loss of hepatocyte function.
FULMINANT HEPATIC FAILURE: A rare, but devastating, syndrome that rapidly progresses within 8 weeks of symptom onset. Normal hepatic function is arrested, and clinical manifestations include markedly elevated serum transaminases, jaundice, coagulopathy, and hepatic encephalopathy.
CLINICAL APPROACH TO VIRAL HEPATITIS
Epidemiology
Most cases of acute hepatitis are caused by infection with one of the five viruses: hepatitis A, B, C, D, or E. These viruses produce virtually indistinguishable clinical syndromes, although it is unusual to observe acute hepatitis C. Affected individuals often complain of a prodrome of nonspecific constitutional symptoms, including fever, nausea, fatigue, arthralgias, myalgias, headache, and sometimes pharyngitis and coryza, which is then followed by the onset of jaundice caused by hyperbilirubinemia and dark urine caused by hyperbilirubinuria. The liver may be enlarged (hepatomegaly) and tender. The clinical course and prognosis vary based on the type of virus causing the hepatitis.
The differential diagnosis for acute hepatitis includes viral, toxic, ischemic, or autoimmune injury. Viral hepatitis can originate from infection by the several viruses described in the material that follows; less commonly, it be caused by Epstein-Barr virus, herpes simplex virus, varicella zoster virus, cytomegalovirus, and adenovirus, among others. Toxic injury may be the result of medications (ie, acetaminophen, statins, phenytoin, ketoconazole), alcohol, supplements (ie, black cohosh, kava), or mushroom poisoning (ie, Amanita phalloides). Ischemic injury may occur during episodes of severe, acute hypoperfusion. Budd-Chiari and veno-occlusive disease may also lead to acute hepatitis. Additional causes include Wilson disease, leptospirosis, malignant infiltration, or heatstroke.
Pathophysiology
Hepatitis A and E both are very contagious and transmitted either by the fecal-oral route, usually through contaminated food or water where sanitation is poor, or from person to person, such as in day care settings by children. Hepatitis A is found worldwide and is the most common cause of acute viral hepatitis in the United States. Hepatitis E is much less common and is found in Asia, Africa, Central America, and the Caribbean. Both hepatitis A and E infections usually lead to self-limited illnesses and generally resolve within weeks. Almost all patients with hepatitis A recover completely and have no long-term complications. Less than 1% of those infected with hepatitis A develop fulminant liver disease resulting in hepatic failure, and those patients are generally > 50 years old and have some underlying chronic liver disease. Most patients with hepatitis E also have uncomplicated courses, but some patients, particularly pregnant women, have been reported to develop severe hepatic necrosis and fatal liver failure.
Hepatitis B is the second most common type of viral hepatitis in the United States and is usually sexually transmitted. It also may be acquired parenterally, such as by intravenous drug use, or during birth from chronically infected mothers. The outcome depends on the age at which the infection was acquired. Up to 90% of infected newborns develop chronic hepatitis B infection, which places the affected infant at significant risk of hepatocellular carcinoma later in adulthood. For individuals infected later in life, approximately 95% of patients will recover completely without sequelae. Between 5% and 10% of patients will develop chronic hepatitis, which may progress to cirrhosis. A chronic carrier state may be seen in which the virus continues to replicate, but it does not cause irreversible hepatic damage in the host.
Hepatitis C is transmitted parenterally by blood transfusions or intravenous drug use and less commonly by sexual contact. The mode of transmission is unknown in approximately 40% of cases. It is uncommonly diagnosed as a cause of acute hepatitis, often producing subclinical infection, but is frequently diagnosed later as a cause of chronic hepatitis with or without the presence of liver cirrhosis. The majority of hepatitis C infection leads to chronic hepatitis, but the development of newer medications can lead to the cure of many patients; for this reason, most preventive guidelines recommend screening for hepatitis C infection at least once during adulthood and more often in high-risk individuals.
Hepatitis D is a defective RNA virus that requires the presence of the hepatitis B virus to replicate. It can be acquired as a coinfection simultaneously with acute hepatitis B or as a later superinfection in a person with a chronic hepatitis B infection. Patients afflicted with chronic hepatitis B virus who then become infected with hepatitis D may suffer clinical deterioration; in 10% to 20% of these cases, individuals develop severe fatal hepatic failure.
Clinical Presentation
Since there are many causes of acute hepatitis, a good history is vital. The history should include targeted questions about the patient’s drug use, sexual contacts, and travel history. Additional questions should investigate possible exposures to toxins and supplements. Timing of symptoms may also help elucidate an etiology.
Examination findings may include jaundice, right upper quadrant tenderness, ascites, and signs of intravascular depletion, such as orthostatic vitals. It is important to perform a complete neurologic examination on the patient to assess for encephalopathy. If encephalopathy is present, then it should be graded I-IV. Grade I may be evident by confusion, abnormal behavior, changes in sleeping patterns, or slurred speech. This may be difficult to distinguish from grade II, which has progressive lethargy. Profound confusion, incoherent speech, and increased sleeping may be signs of grade III encephalopathy, while grade IV is hallmarked by coma. Findings on physical examination may not help distinguish the etiology of acute hepatic failure, and further studies are usually needed.
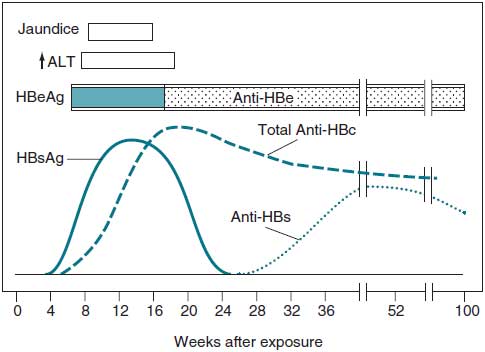
Serologic studies are generally used to establish a diagnosis. Anti-hepatitis A immunoglobulin M (IgM) establishes an acute hepatitis A infection. Anti-hepatitis C antibody is present in acute hepatitis C, but the test result may be negative for several weeks. The hepatitis C RNA assay, which becomes positive earlier in the disease course, often aids in the diagnosis. Acute hepatitis B infection is diagnosed by the presence of hepatitis B surface antigen (HBsAg) in the clinical context of elevated serum transaminase levels and jaundice. HBsAg later disappears when the antibody (anti-HBs) is produced (Figure 26–2). There is often an interval of a few weeks between the disappearance of HBsAg and the appearance of anti-HBsAb. This period is referred to as the “window period.” During this interval, the presence of anti-hepatitis B core antigen IgM (anti–HBc IgM) is indicative of an acute hepatitis B infection. A positive hepatitis B precore antigen (HBeAg) represents a high level of viral replication and high infectivity. It is almost always present during acute infection, but its persistence after 6 weeks of illness is a sign of chronic infection and high infectivity. Persistence of HBsAg or HBeAg is a marker for chronic hepatitis or a chronic carrier state; elevated versus normal serum transaminase levels distinguish between these two entities, respectively. Patients who have been vaccinated against hepatitis B will have a positive HBsAb but no other positive serology.
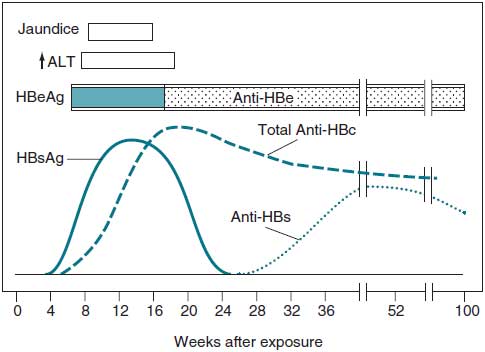
Figure 26–2. Serologic markers in acute hepatitis B infection. Note: Total Anti-HBc = both IgG and IgM. (Reproduced with permission, form Braunwald E, Fauci AS, Kasper DL, et al, eds. Harrison’s Principles of Internal Medicine, 16th ed. 2005. Copyright © McGraw Hill LLC. All rights reserved.)
Treatment and Complications
Fortunately, in most cases of acute viral hepatitis, patients recover completely, so the treatment is generally supportive. However, fulminant hepatic failure due to massive hepatic necrosis may progress over a period of weeks and is usually caused by infections from the hepatitis B and D viruses or from toxins. Toxin- or drug-induced liver injury is the most common cause of acute liver failure and can be a result of direct toxic effects of substances on the liver parenchyma (acetaminophen, A. phalloides) or idiosyncratic reactions of medications (halothane, isoniazid, phenytoin). Direct toxic effects are predictable and dose dependent, but idiosyncratic reactions are not.
Acute hepatic failure is characterized by rapid progression of encephalopathy from confusion or somnolence to coma. Patients also have markedly high serum aminotransferase levels, worsening coagulopathy, rising bilirubin levels, ascites and peripheral edema, hypoglycemia, hyperammonemia, and lactic acidosis. Fulminant hepatic failure carries a poor prognosis (the mortality for comatose patients is 80%) and often is fatal without an emergent liver transplant.
Prevention. The efficacy of the hepatitis A vaccine (available in two doses given 6 months apart) exceeds 90%. It is indicated for individuals planning to travel to endemic areas, along with those with chronic hepatitis B or C. Postexposure prophylaxis with hepatitis A immunoglobulin, along with the first injection of the vaccine, should be given to household and intimate contacts within 2 weeks of exposure. The hepatitis B vaccine (given in three doses over 6 months) provides effective immunity in more than 90% of patients. It is recommended for health care workers, those with chronic hepatitis C, and all infants in the United States. Hepatitis B immunoglobulin (HBIg) is given after exposure, such as to health care providers after a needlestick injury from an infected patient, or to newborns of infected mothers. The first inoculation of the vaccine is usually given concurrently. There is no immunization and no proven postexposure prophylaxis for persons exposed to hepatitis C. Interferon and nucleos(t)ide analogs, such as entecavir, tenofovir, or lamivudine, are used to treat patients with chronic hepatitis B. Treatment for chronic hepatitis C has undergone major advancement with utilization of direct acting antivirals (DAAs), sometimes in combination with ribavirin or interferon, allowing for high rates of curative treatment of chronic hepatitis C. Examples of DAA selections include sofosbuvir, a nucleoside analog of the hepatitis C virus, and simeprevir, a protease inhibitor specific to proteins on the hepatitis C virus. Regimens for treatment are based on hepatitis C genotyping, with genotype I being the most common, along with history of prior treatment failure and comorbidities.
CLINICAL APPROACH TO ACETAMINOPHEN HEPATITIS
Pathophysiology
Acetaminophen poisoning is among the most common types of medication-induced toxicity and death. Acetaminophen-induced hepatocellular injury may result after a single, large ingestion, as in a suicide attempt, or by chronic use of over-the-counter acetaminophen-containing preparations for treatment of pain or fever. Hepatic toxicity most often occurs after an acute ingestion of 10 g or more, but lower doses (4 g in 24 hours) may cause injury to patients with preexisting liver disease, particularly in those who abuse alcohol. Acetaminophen is metabolized in the liver by the cytochrome P450 enzyme system, which produces a toxic metabolite. This metabolite is detoxified by binding to glutathione. Risk of hepatic injury is greater when P450 activity is augmented by drugs such as ethanol or phenobarbital or when less glutathione is available, as in alcoholism, malnutrition, or acquired immunodeficiency syndrome (AIDS). Acetaminophen levels are measured between 4 and 24 hours after an acute ingestion and plotted on a nomogram to predict possible hepatotoxicity and determine if treatment is necessary. Sometimes, empiric therapy is started even before laboratory results return.
Treatment
Treatment of the acetaminophen toxicity is dependent on time of presentation. Patients who present promptly after ingestion of large amounts of acetaminophen may benefit from gastric decontamination with charcoal if no additional contraindications exist. Gastric decontamination is most beneficial if performed within the first 4 hours after ingestion. If acetaminophen levels are above the level that predisposes to hepatic injury or if there is a significant risk of hepatotoxicity, administration of NAC is indicated. NAC functions as an antidote to acetaminophen toxicity by providing cysteine to replenish glutathione stores. Ideally, NAC should be started prior to evidence of liver injury and within the first 10 hours of ingestion in attempt to prevent liver damage; it is continued for 72 hours. Meanwhile, the patient should not receive any medications that are known to be hepatotoxic. It is equally important to ensure that patients are receiving adequate supportive therapy based on the severity of disease presentation. Patients may require fluid resuscitation, airway support, vasopressors, dialysis, and/or management of cerebral edema.
CASE CORRELATION
- See also Case 24 (Liver Cirrhosis, Probably Alcoholic) and Case 27 (Painless Jaundice, Pancreatic Cancer).
COMPREHENSION QUESTIONS
26.1 A 25-year-old medical student is stuck with a hollow needle during a procedure performed on a patient known to have hepatitis B and C viral infections, but who is HIV negative. The student’s baseline laboratory studies include serology: HBsAg negative, anti-HBsAb positive, and anti-HBc IgG negative. Which of the following regarding this medical student’s hepatitis status is true?
A. Prior vaccination with hepatitis B vaccine
B. Acute infection with hepatitis B virus
C. Prior infection with hepatitis B virus
D. The student was vaccinated for hepatitis B but is not immune
26.2 What postexposure prophylaxis (if any) should the student described in Question 26.1 receive?
A. HBIg
B. Oral tenofovir
C. Immunoglobulin
D. Reassurance
26.3 In a suicide attempt, an 18-year-old woman took 4 g of acetaminophen, approximately 8 hours previously. On examination, she is drowsy but oriented and answers questions appropriately. Her blood pressure is 120/70 mm Hg and heart rate is 90 bpm. She is anicteric. Her heart, lung, and abdominal examinations are normal. Her acetaminophen level is 30 mcg/mL. Which of the following is the best next step to be performed for this patient?
A. Immediately start NAC
B. Observation
C. Alkalinize the urine
D. Administer intravenous activated charcoal
ANSWERS
26.1 A. This student’s serology is most consistent with vaccination and not prior infection. Like all health care workers, the student should have been vaccinated against the hepatitis B virus, which induces anti-HBs IgG antibody, and is thought to be protective. Not all people receiving the vaccine develop an adequate antibody titer; if none were detected, it would indicate the need for revaccination (answer D). Patients with prior hepatitis B infection (answer C) also have anti-HBsAb but will additionally have anti-HBc IgG. Acute infection (answer B) would be established by the presence of either HBsAg or anti-HBc IgM.
26.2 D. No postexposure prophylaxis is definitively indicated. The student has detectable protective antibody levels against the hepatitis B virus, and if the levels are judged to be adequate, the student is protected against infection. Thus, the key point in this question is that the presence of anti-HBsAg antibody is protective. Oral tenofovir (answer B) is a treatment for chronic hepatitis B infection and is part of an antiretroviral prophylaxis if the patient were HIV positive. There is no effective prophylaxis for hepatitis C exposure. Seroconversion against this virus needs to be retested at a later time. Thus, passive immunization with HBIg (answer A) is not needed. Answer C (immunoglobulin) is indicated for hepatitis A exposure but not hepatitis B.
26.3 B. The serum acetaminophen level of 30 mcg/mL, with last ingestion 8 hours previously, is plotted on the nomogram and falls below the “danger zone” of possible hepatic injury. Thus, this patient should be observed. Sometimes, patients will take more than one medication, and serum and/or urine drug testing may be worthwhile. Gastrointestinal activated charcoal, not intravenous charcoal (answer D), is used for other ingestions. Initiation of NAC (answer A) is recommended when the normogram suggests possible hepatic injury. Alkalinization (answer C) of the urine is helpful to enhance excretion of acidic toxins such as aspirin but does not have a role in acetaminophen toxicity.
CLINICAL PEARLS
▶ The most common cause of acute hepatic failure is toxin or drug injury, which may be due to direct toxic effects or an idiosyncratic reaction.
▶ The likelihood of toxic acetaminophen injury and the need for treatment can be predicted from a nomogram based on serum level and the time since last ingestion.
▶ The majority of adults with acute hepatitis B infection recover completely. However, 5% to 10% develop chronic hepatitis.
▶ Vaccination for hepatitis B should produce measurable HBsAb. Presence of anti-HBc IgG indicates evidence of prior infection. Anti-HBc IgM can be positive during the “window period” of acute infection.
▶ Prevention of hepatitis B viral infection hinges on long-term immunity with a highly effective recombinant vaccine or postexposure pro-phylaxis with HBIg. There is no vaccine or postexposure prophylaxis for hepatitis C.
REFERENCES
Bass NM. Toxic and drug-induced liver disease. In: Cecil RL, Bennett JC, Goldman L, eds. Cecil’s Textbook of Medicine. 21st ed. Philadelphia, PA: Saunders; 2000:781-782.
Chiew AL, Gluud C, Brok J, Buckley NA. Interventions for paracetamol (acetaminophen) overdose. Cochrane Database Syst Rev. 2018;23(2):CD003328.
Chopp S, Vanderwall R, Hult A, Klepser M. Simeprevir and sofosbuvir for treatment of hepatitis C infection. Am J Health Syst Pharm. 2015;17:1445-1455.
Deinstag JL. Acute viral hepatitis. In: Jameson JL, Fauci AS, Kasper, DL, et al, eds. Harrison’s Principles of Internal Medicine. 20th ed. New York, NY: McGraw Hill; 2018:2357-2557.
Dienstag JL. Toxic and drug-induced hepatitis. In: Jameson JL, Fauci AS, Kasper, DL, et al, eds. Harrison’s Principles of Internal Medicine. 20th ed. New York, NY: McGraw Hill; 2018:2558-2566.
Friedman LS. Approach to the patient with abnormal liver biochemical and function tests. Chopra S, ed. UpToDate. Waltham, MA: UpToDate; 2019. http://www.uptodate.com/contents/approach-to-the-patient-with-abnormal-liver-biochemical-and-function-tests. Accessed July 28, 2019.
Heard K, Dart R. Acetaminophen (paracetamol) poisoning in adults: treatment. Traub ST, ed. UpToDate. Waltham, MA: UpToDate; 2019. http://www.uptodate.com/contents/acetaminophen-paracetamol-poisoning-in-adults-treatment. Accessed July 5, 2019.
Lawitz E, Mangia A, Wyles D, et al. Sofosbuvir for previously untreated chronic hepatitis C infection. N Engl J Med. 2013;368:1878-1887.
Luis S, Marsano MD. Hepatitis. Prim Care Clin Office Pract. 2003;30:81-107.
Recommendations for testing, managing, and treating hepatitis C. Joint panel from the American Association of the Study of Liver Diseases and the Infectious Diseases Society of America. http://www.hcvguidelines.org/. Accessed July 7, 2019.


0 comments:
Post a Comment
Note: Only a member of this blog may post a comment.