Acute Diverticulitis Case File
Eugene C. Toy, MD, Gabriel M. Aisenberg, MD
Case 22
A 61-year-old man comes to the emergency center complaining of 3 days of worsening abdominal pain. The pain is localized to the left lower quadrant of his abdomen. It began as an intermittent crampy pain and now has become steady and moderately severe. He feels nauseated, but he has not vomited. He had a small loose stool at the beginning of this illness, but he has had not had any bowel movements over past 2 days. He has never experienced these symptoms before, and he does not have any history of gastrointestinal (GI) illnesses.
On examination, his temperature is 100.2 °F, heart rate is 98 beats per minute (bpm), and blood pressure is 110/72 mm Hg. He has no pallor or jaundice. His chest is clear, and his heart rhythm is regular without murmurs. His abdomen is mildly distended with hypoactive bowel sounds and marked left lower quadrant tenderness with voluntary guarding. Rectal examination reveals tenderness, and his stool is negative for occult blood.
Laboratory studies are significant for a white blood cell count of 12,800/mm3 with 74% polymorphonuclear leukocytes, 22% lymphocytes, and a normal hemoglobin and hematocrit. A plain film of the abdomen shows no pneumoperitoneum and a nonspecific bowel gas pattern.
▶ What is the most likely diagnosis?
▶ What are risk factors for developing this condition?
▶ What are the most appropriate next steps in management?
ANSWERS TO CASE 22:
Acute Diverticulitis
Summary: A 61-year-old man presents with
- A 3-day history of worsening new-onset abdominal pain
- Low-grade fever
- Abdominal distention, hypoactive bowel sounds, and voluntary guarding
- Leukocytosis with normal hemoglobin and no occult blood
- Normal x-ray of the abdomen
Most likely diagnosis: Acute sigmoid diverticulitis.
Risk factors: Frequent red meat consumption, Western diet, and low-fiber diets.
Most appropriate next steps: This patient shows voluntary guarding, which is concerning for peritoneal inflammation, likely due to complicated diverticulitis. The patient should be admitted to the hospital for intravenous antibiotics, imaging, and close monitoring. Computed tomographic (CT) scan of the abdomen will be very useful to confirm the diagnosis and to exclude pericolic abscess or other complications, such as fistula formation.
- Describe the complications of diverticular disease. (EPA 1, 10)
- Recognize the appropriate therapy of acute diverticulitis, which is dependent on the age of the patient and the severity of the disease presentation. (EPA 1, 4)
- List the complications of diverticulitis and the indications for surgical intervention. (EPA 4, 10)
- Differentiate between inpatient and outpatient management of diverticulitis. (EPA 1, 2, 9)
- Discuss strategies for prevention and follow-up in acute diverticulitis. (EPA 7, 12)
Considerations
This 61-year-old man presents with new-onset, progressively worsening, severe, lower left abdominal pain. The most likely diagnosis is acute diverticulitis, but the differential diagnosis for these symptoms is broad; several key diagnoses that carry significant morbidity and mortality for the patient must be excluded. These include bowel perforation, ischemic colitis, and colon cancer. This patient had an x-ray that showed no free air in the abdomen. This makes pneumoperitoneum secondary to bowel perforation, which is a surgical emergency, less likely. Ischemic colitis is another diagnostic consideration in an older patient, but it usually is associated with signs of bleeding and a history of atherosclerotic disease and pain out of proportion to the physical examination findings. As colon cancer can present with abdominal pain and bleeding per rectum, the patient must receive age-appropriate colon cancer screening once acute diverticulitis has resolved.
APPROACH TO:
Diverticulitis
COLONIC DIVERTICULUM: Herniation of the mucosa and submucosa through a weakness of the muscle lining of the colon.
DIVERTICULITIS: Inflammation of a colonic diverticulum, typically on the left colon, such as the sigmoid.
DIVERTICULOSIS: Presence of diverticular disease in the colon without inflammation; it is often asymptomatic or may present with painless bright red rectal bleeding.
RECURRENT DIVERTICULITIS: Subsequent diverticulitis episode(s) after the resolution of the first attack of acute diverticulitis, which may not be as severe.
SMOLDERING DIVERTICULITIS: Symptomatic, uncomplicated diverticulitis that persists after the initial episode and is refractory to medical treatment.
CLINICAL APPROACH
Pathophysiology
Diverticulosis is extremely common, affecting 50% to 80% of people older than 80 years. Colonic diverticula are, in fact, pseudodiverticula through weakness in the muscle lining, typically at areas of vascular penetration to the smooth muscle. Therefore, their walls do not contain the muscle layers surrounding the colon. They are typically 5 to 10 mm in diameter and occur mainly in the distal colon. The development of diverticula has been linked to insufficient dietary fiber, leading to a slower colonic transit and increased resting colonic intraluminal pressure. Most patients will remain asymptomatic. Some patients, however, will have chronic symptoms (eg, nonspecific lower abdominal pain aggravated by eating and relieved upon defecation, bloating, constipation, or diarrhea) resembling those of irritable bowel syndrome. A patient with diverticulosis may even present with acute symptoms that could be confused with acute diverticulitis, but upon further workup there is no evidence of inflammation. This entity has been named “painful diverticular disease without diverticulitis.”
Acute diverticulitis is a common complication of diverticulosis, developing in approximately 20% of all patients with diverticula. The risk of diverticulitis is increased in patients who use medications such as aspirin and nonsteroidal
anti-inflammatory drugs, patients who are obese, or those who lead sedentary lifestyles. Patients often present with acute abdominal pain and signs of peritoneal irritation localizing to the left lower quadrant, often presenting like “left-sided appendicitis.” Inspissated stool particles (fecaliths) appear to obstruct the diverticular neck, causing more inflammation and diminished venous outflow, as well as bacterial overgrowth, which ultimately leads to abrasion and perforation of the thin diverticular wall. Most cases are uncomplicated and may be medically managed in an outpatient setting, but 25% of cases develop complications that may require hospitalization or surgical intervention (Table 22–1).
Clinical Presentation
Patients usually present with visceral pain that localizes later to the left lower quadrant and may be associated with fever, nausea, vomiting, dysuria, diarrhea, or constipation. A right lower quadrant presentation would not exclude this diagnosis because diverticulitis can also affect the ascending colon or cecum. On examination, the patient may have localized left lower quadrant tenderness or more diffuse abdominal tenderness with peritoneal irritation signs, such as guarding or rebound tenderness. The patient may also have a palpable mass or abdominal distension on examination. On rectal examination, the patient may exhibit tenderness if there is an abscess present. Laboratory testing will show neutrophil-predominant leukocytosis.
Plain film radiographs, including abdominal erect and supine films with a chest x-ray, are routinely performed but usually are not diagnostic. These films can help to identify patients with pneumoperitoneum and assess their cardiopulmonary status, especially in patients with other comorbid conditions. Barium enemas are contraindicated for fear of perforation and spillage of contrast into the abdominal cavity, a catastrophic complication. Endoscopy is also relatively contraindicated in the acute phase due to risk of perforation and usually is reserved for use at least 6 weeks after resolution of the acute episode. The purpose of the colonoscopy is to confirm the presence of diverticuli and to exclude colonic neoplasia.
CT scan is typically the preferred modality of choice for diagnosing diverticulitis. Findings consistent with diverticulitis include inflamed sigmoid diverticula, thickening of the bowel wall to more than 4 mm, pericolic fat stranding signifying inflammation, or the finding of a diverticular abscess. Although these findings have high specificity for diverticulitis, they have low sensitivity, and only 50% of patients will have these characteristics on CT. Pregnant patients can undergo ultrasonography to avoid the harmful effects of ionizing radiation to the fetus.
Treatment
Outpatient Therapy. Patients with uncomplicated diverticulitis can usually be managed conservatively with bowel rest and antibiotics. Select patients with less severe presentation, ability to tolerate oral antibiotic medications, and absence of significant comorbid conditions may be managed as outpatients. There is weak evidence supporting the use of antibiotic therapy in uncomplicated diverticulitis. Several studies showed that antibiotics do not affect recovery time or prevent future complications in uncomplicated diverticulitis. However, antibiotics are often prescribed as a part of the standard practice. Antibiotic therapy should cover a broad spectrum and should especially target gram-negative rods and anaerobes. Oral antibiotics may include a quinolone plus metronidazole, or amoxicillin-clavulanate for 7 to 10 days. Patients should be instructed to take clear liquids only and advance their diet slowly only if clinical improvement is evident after 2 to 3 days.
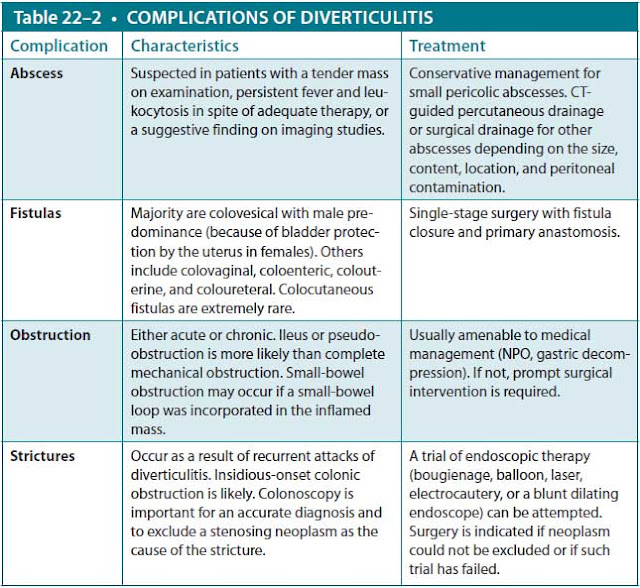
Inpatient Therapy. Factors that advocate for inpatient therapy include elderly or immunosuppressed patients, those with significant comorbidities, those with high fever or significant leukocytosis, and those in need for narcotics to control pain. Patients requiring hospitalization can be treated with clear liquids or given nothing by mouth (NPO) with intravenous hydration, depending on the severity of symptoms. Intravenous empiric antibiotics with broad-spectrum activity against gram-negative rods and anaerobic organisms such as piperacillin/tazobactam or ceftriaxone plus metronidazole should be started. Pain, fever, and leukocytosis are expected to diminish with appropriate management in the first few days of treatment, at which point the dietary intake can be advanced gradually. CT imaging is indicated to identify complications (Table 22–2), such as abscess, stricture, or obstruction in the patient with persistent fever or pain. The patient can be discharged once able to tolerate an oral diet, their vital signs are stable, and their abdominal pain has resolved.
Surgical Therapy. Surgical management such as sigmoid resection is indicated for low surgical risk patients with complicated diverticulitis. Patients who have suffered two or more episodes of uncomplicated diverticulitis are often treated surgically, but medical management may also be continued without increased risk of perforation. Indications for emergent surgical intervention include generalized peritonitis, uncontrolled sepsis, perforation, and clinical deterioration. Surgical interventions include abdominal washout, CT-guided percutaneous drainage of abscesses, and bowel resection.
Prevention and Recurrence. Once the acute phase has resolved, medical management to prevent symptoms includes a high-fiber diet, anti-inflammatory medications such as mesalamine for chronic low-grade inflammation, and probiotics. Treatment of diverticulosis consists of changing dietary habits, especially increasing fiber intake. Avoidance of nuts or foods with small seeds (eg, strawberries) is traditionally advised, although data supporting this recommendation is lacking. Patients should be encouraged to exercise routinely and counseled to stop smoking. Colonoscopy is commonly performed at least 6 weeks after an attack of diverticulitis to evaluate for colorectal carcinoma, which may mimic the clinical presentation of diverticulitis.
Abbreviations: CT, computed tomography; NPO, nothing by mouth.
Some patients may continue to have symptoms after an initial attack, leading to a subacute phase called “smoldering diverticulitis.” These patients may develop chronic symptoms that last longer than 6 months without progressing to acute diverticulitis or other complications. About a third of the patients with one episode of diverticulitis will develop recurrent disease. Though those with uncomplicated diverticulitis are not at increased risk of recurrence, patients with complicated disease are 1.5 times more likely to develop recurrence. Patients without significant other comorbidities who have chronic smoldering diverticulitis or recurrent or complicated diverticulitis should be offered surgical intervention.
Complications
Complications include hemorrhage and obstruction. Diverticular hemorrhage is the most common cause of hematochezia in patients older than 60 years and typically presents as painless passage of bright red blood. Only 20% of patients with diverticulosis will experience GI bleeding. Generally, hemorrhage is abrupt in onset and resolution. The diagnosis may be established by finding diverticula on colonoscopy without other pathology. Most diverticular hemorrhages are self-limited, and treatment is supportive, with intravenous fluid or blood product transfusion as needed. For patients with recurrent or chronic bleeding, resection of the affected colonic segment may be indicated. Bowel obstruction is rare and can be due to acute inflammation leading to partial obstruction of the bowel lumen or, less commonly, chronic inflammation leading to stricture formation. Sometimes surgical therapy is needed if medical treatment is ineffective.
CASE CORRELATION
- See also Case 20 (Peptic Ulcer Disease), Case 21 (Colitis and Inflam-matory Bowel Disease), Case 23 (Chronic Diarrhea), and Case 25 (Pancreatitis/Gallstones).
COMPREHENSION QUESTIONS
22.1 A 48-year-old woman is admitted to the hospital with left lower quadrant abdominal pain, leukocytosis, and a CT scan showing sigmoid wall thickening consistent with a pericolic abscess. Her medical history is significant for a similar hospitalization with the same diagnosis less than 1 year previously. Which of the following is the most appropriate next step in management?
A. Surgical consultation for exploratory laparotomy and sigmoid resection
B. Intravenous antibiotics and colonoscopy for evaluation for colon cancer
C. Intravenous antibiotics and barium enema to evaluate for possible colonic malignancy
D. Intravenous antibiotics and recommendations for postdischarge diet high in fiber with whole grains and nuts to minimize the risk of diverticular progression
22.2 A 78-year-old is woman is hospitalized for a 2-day history of progressive fever and chills, decreased mentation, and lower abdominal pain. On examination, her blood pressure is 120/70 mm Hg, heart rate is 110 bpm, and temperature is 101 °F. Examination shows severe right lower quadrant abdominal tenderness and guarding. Which of the following is the most likely diagnosis?
A. Ruptured diverticulitis
B. Meningitis
C. Ruptured appendicitis
D. Ischemic bowel
E. Sepsis secondary to urinary tract infection
22.3 A 58-year-old man presents to the emergency room for evaluation of a 2-day history of left lower quadrant abdominal pain. The patient notes that during this time he has had fevers, chills, and constipation. His vital signs show a temperature of 102 °F, pulse of 90 bpm, and respiratory rate of 20 breaths/min. Physical examination shows abdominal pain localizing to the left lower quadrant and mild rebound tenderness. There are no abnormalities on cardiopulmonary examination. Which of the following diagnostic tests is the best next step?
A. Barium enema
B. Flexible sigmoidoscopy
C. CT imaging of the abdomen
D. Laparoscopic examination
E. Observation
22.4 A 74-year-old man presents to the emergency room due to severe abdominal pain that started 2 hours ago. He has had three bloody stools during this time. The patient has a past medical history of diabetes mellitus, hypertension, hyperlipidemia, and coronary artery disease. He recalls that he recently had heart surgery to repair a vessel with a weak wall. He has a 30 pack-year history of smoking but quit several years ago. His diet consists of red meats and low fiber. He drinks one or two glasses of wine a week. The patient’s temperature is 101.2 °F, pulse is 110 bpm, and blood pressure is 90/58 mm Hg. On physical examination, his abdomen is distended and diffusely tender to palpation. Bowel sounds are absent. What is the likely etiology of this patient’s condition?
A. Inflammation of herniated colonic wall mucosa
B. Ischemia and necrosis of the watershed areas of the colon
C. GI bleed due to arteriovenous malformation
D. Neoplasia of columnar epithelium in the colon
22.5 An 85-year-old woman presents to the emergency department with severe left lower abdominal pain that began several hours ago. The patient has a past medical history of hypertension, osteoporosis, and rheumatoid arthritis. She was brought in by a caretaker at a nursing home. The patient’s temperature is 103.8 °F, pulse is 115 bpm, and blood pressure is 135/80 mm Hg. She is mildly confused but alert and answers questions. Her heart and lung examinations are normal. Abdominal examination shows tenderness to palpation of the left lower quadrant with guarding, but no peritoneal signs. Her hemoglobin is 11.2 g/dL, leukocyte count is 14,000/mm3, and platelet count is 280,000/mm3. What is the best next step in the management of this patient?
A. Outpatient management, oral amoxicillin-clavulanate, and follow-up in 2 to 3 days
B. Outpatient management, no antibiotics, and bowel rest
C. Inpatient management, oral amoxicillin-clavulanate, and NPO with intravenous hydration
D. Inpatient management, intravenous piperacillin/tazobactam, and NPO with intravenous hydration
ANSWERS
22.1 A. This patient has complicated diverticulitis, with recurrent disease (as defined by two or more complicated episodes); she is a low surgical risk and thus should be evaluated for resection. Barium enema (answer C) is contraindicated due to risk of perforation, and dietary recommendations regarding nuts and seeds (answer D) are unsupported by data. Colonoscopy (answer B) should be postponed until at least 6 weeks after the acute case of diverticulitis to avoid perforation.
22.2 C. This patient has right lower abdominal tenderness and fever, which is most likely due to acute appendicitis. The most common cause of an acute abdomen at any age is appendicitis. Ischemic bowel (answer D) usually presents with severe abdominal pain out of proportion to abdominal examination findings and often with a history of atherosclerotic vascular disease. Sepsis due to a urinary tract infection (answer E) is a common cause of septic shock and hypotension, but it usually does not cause abdominal findings; flank tenderness or merely generalized sepsis is more common.
22.3 C. CT imaging is the modality of choice in evaluating diverticulitis. Barium enema (answer A) and endoscopy tend to increase intraluminal pressure and can worsen diverticulitis or lead to colonic rupture. Colonoscopy and flexible sigmoidoscopy (answer B) are also contraindicated in the acute setting and should be delayed until 6 weeks after to rule out a neoplasm. Observation (answer E) is not appropriate in this patient before a complete evaluation is performed.
22.4 B. This patient has ischemic colitis, which is suggested by his acute presentation of bloody stools, diffuse abdominal pain, absent bowel sounds, and hypotension. This patient has several risk factors for ischemic colitis, such as coronary artery disease and history of aortic aneurysm repair (weakening of vessel wall). Although arteriovenous malformation (answer C) and angiodysplasia are common causes of lower GI bleeds, they do not usually present with severe abdominal pain and shock, and the patient usually has a history of renal disease. Colorectal cancer (answer D) is a chronic condition that may present with lower GI bleed, anemia, changes in bowel habits, and weight loss.
22.5 D. This elderly patient is quite ill. Although her current blood pressure is normal, her temperature of 103.8 °F, tachycardia, and leukocytosis portend serious illness. The patient should be admitted to the hospital for inpatient management. The physical findings point toward an abdominal process. Regardless of the etiology, this patient should be treated within 1 hour (optimally after blood and urine cultures). Treatment includes intravenous antibiotics that are broad spectrum and target gram-negative rods as well as anaerobic bacteria, intravenous fluids, and serum lactate level. A CT scan of the abdomen is important to assess the etiology of the abdominal pain and decide appropriate therapy based on the findings. Answers A and B (outpatient treatment) are not appropriate options for this patient due to the seriousness of the infection. Similarly, oral antibiotics (answer C) are not acceptable due to the patient’s condition.
CLINICAL PEARLS
▶ Acute diverticulitis usually presents with left lower quadrant pain, fever, leukocytosis, and constipation and often with signs of peritoneal inflammation.
▶ Inpatient management of diverticulitis is indicated in patients with complications such as peritonitis, abscess, and strictures or in patients who are at high risk of morbidity and mortality.
▶ Some patients can be managed on an outpatient basis and should be reevaluated in 2 to 3 days to monitor resolution of symptoms.
▶ Uncomplicated diverticulitis can be treated medically with antibiotics and bowel rest.
▶ Diverticulitis can be complicated by perforation with peritonitis; pericolic abscess; fistula formation, often to the bladder; and strictures with colonic obstruction. Complicated diverticulitis may require hospitalization, intravenous antibiotics, and possibly surgical intervention.
▶ Enemas and endoscopy are usually avoided in the acute setting because of the risk of perforation.
▶ Prevention includes incorporation of dietary fiber, eating less meat, smoking cessation, and routine exercise.
REFERENCES
Ahmed R, Gearhart SL. Diverticular disease and common anorectal disorders. In: Jameson JL, Fauci AS, Kasper SL, et al, eds. Harrison’s Principles of Internal Medicine. 20th ed. New York, NY: McGraw Hill Education; 2018:1971-1978.
Ferzoco LB, Raptopoulos V, Silen W. Acute diverticulitis. N Engl J Med. 1998;338:1521-1526.
Pemberton JH. Acute colonic diverticulitis: medical management. Weiser M, Chen W, ed.
UpToDate. Waltham, MA: UpToDate; 2019. https://www.uptodate.com/contents/acute-colonic-diverticulitis-medical-management. Accessed June 16, 2019.
Stollman N, Raskin J. Diverticular disease of the colon. J Clin Gastroenterol. 1999;29:241-252.
Wilkins T, Embry K, George R. Diagnosis and management of acute diverticulitis. Am Fam Physician. 2013;87(9):612-620.


0 comments:
Post a Comment
Note: Only a member of this blog may post a comment.