Delirium from Hepatic Encephalopathy Case File
Eugene C. Toy, MD, Ericka Simpson, MD, Pedro Mancias, MD, Erin E. Furr-Stimming, MD
CASE 9
A 63-year-old woman is brought into the emergency department (ED) with altered mental status. Her family tells you that the patient was in her normal state of health until 3 days ago and since has become sleepier and more confused. She is a very private person and has never told her children about any health problems. The family does confide that the patient was an alcoholic for many years, but her doctor recently convinced her to stop drinking because it was “damaging her organs.” On interview, the patient answers most questions inappropriately and with anger; however, at times she answers lucidly. She denies experiencing any headache, neck pain, visual symptoms, or loss of balance. On examination, she is afebrile, her blood pressure is 124/78 mm Hg, and her pulse is 100 beats/min. She is awake but inattentive, and her focus waxes and wanes throughout the examination. Her general examination is notable for the absence of nuchal rigidity, no obvious head trauma, and a distended abdomen. Her Mini-Mental State Examination (MMSE) is 24/30 and she is having difficulty with orientation, concentration, and recall. She fluctuates with being appropriate throughout the examination. She does not have any aphasia or dysarthria but is circumstantial and tangential. Her neurologic examination is significant for grossly intact cranial nerves and intact pinprick sensation to the face. The remainder of the sensory, motor, and cerebellar examination cannot be fully assessed because she is uncooperative with much of the examination. The tests she does tolerate are largely normal; however, when asked to bend her wrists upward, she finds it difficult due to involuntary flapping with loss of tone in the wrist extensors.
▶ What is the most likely diagnosis?
▶ What is the next diagnostic step?
ANSWERS TO CASE 9:
Delirium from Hepatic Encephalopathy
Summary: A 63-year-old woman with a history of alcohol abuse presents with an alteration in mental status, which developed over 3 days. Her mental status shows attention deficits, disorganized thinking, altered psychomotor activity, difficulty focusing, memory deficits, and disorientation. Additionally, it seems that there has been some fluctuation of her symptoms. The examination is notable for absent nuchal rigidity, a distended abdomen, and flapping movements at the wrists.
- Most likely diagnosis: Delirium from hepatic encephalopathy.
- Next diagnostic step: Computed tomography (CT) scan of the head, complete blood count (CBC), comprehensive metabolic panel, blood alcohol level, and urine toxicology screen
ANALYSIS
Objectives
- Be familiar with the clinical presentation of delirium.
- Learn the differential diagnosis of delirium.
- Describe how to evaluate a patient with delirium.
Considerations
This 63-year-old woman presents with acute fluctuating levels of attention,
confusion, and altered psychomotor activity developing over 3 days. The findings of attentional deficits, disorganized thinking, altered psychomotor activity, difficulty focusing, memory deficits, and disorientation are characteristic for delirium when there is a waxing and waning of symptoms and a relatively acute onset. Importantly, not all patients with altered mental status have delirium. The hallmarks of delirium are cognitive impairment, impaired attention, and fluctuating course. The differential of altered mental status can be quite broad and must first be accurately defined. Given the history of chronic alcoholism, a distended abdomen (likely ascites) and flapping hand motions (likely asterixis), her presentation is suggestive of hepatic encephalopathy. This occurs when there is an accumulation of harmful neurotoxic substances such as ammonia and manganese that would otherwise be removed by a healthy liver.
APPROACH TO:
Delirium
DEFINITIONS
DELIRIUM: A neurobehavioral disorder with a fluctuating course including inattention and acute alteration in mental status.
ATTENTION: The ability to focus on specific stimuli while excluding others.
ASTERIXIS: A type of negative myoclonus or loss of muscle tone in the wrist extensors, resulting in a characteristic flapping motion. It is classically caused by hyperammonemia in liver disease and can be linked to various metabolic conditions.
CLINICAL APPROACH
The presentation of acute mental status change, abnormal attention, and a fluctuating course should alert the clinician to delirium. Delirium is a disorder caused by many different etiologies and is the most common neurobehavioral disorder in hospitals. It has been reported that up to 40% of hospitalized patients in intensive care units (ICUs) have delirium. There are various recognized risk factors for delirium, the most common being age (particularly >80 years), preexisting cognitive impairment, dehydration, electrolyte disturbances, and gender (men more so than women). Patients admitted to hospitals with delirium account for 10% to 24% of all admissions, with up to 26% of these resulting in death. Almost 80% of patients will experience delirium near the time of death.
The pathophysiology of delirium is not well established, but there is evidence to suggest that there are multiple neurotransmitter abnormalities affecting acetylcholine, dopamine, and serotonin levels that lead to reversible impairment of cerebral oxidative metabolism. There is also an inflammatory component to the mechanism of delirium, with some studies showing that cytokines such as interleukin-1 and interleukin-6 are upregulated. The central nervous system (CNS) pathways involved in delirium are not well established; however, the ascending reticular formation in the upper brainstem, prefrontal cortex, posterior parietal cortex, and the thalamus all seem to be involved.
Clinical characteristics of delirium include an acute change in mental status with a fluctuating course, disorganized thinking, and attentional deficits. Other risk factors are listed in Table 9–1. Delirium should be differentiated from dementia, which is usually marked by a slow-onset, chronic cognitive disorder.
Diagnosis
The diagnosis of delirium is clinical, with an emphasis on evaluating level of attention. Attention can be evaluated by serial reversal test (such as asking the patient to spell a word backward). The history should include a review of medications the patient is taking and information obtained from friends or family. The neurologic examination may be nonfocal, although patients may have dysarthria, tremor, various motor abnormalities, or asterixis (loss of tone with passive extension of wrist).
Laboratory evaluation should include a comprehensive metabolic panel with close attention to electrolyte levels, glucose, blood urea nitrogen (BUN), liver function studies, a CBC to evaluate for infection, thyroid function studies, and ammonia levels. Arterial blood gas (ABG) or pulse oximetry should be obtained, especially if the patient has a history of lung disease or smoking. Urine toxicology studies in those individuals with a history of drug abuse or at risk for drug abuse should be obtained as well. A CT scan of the head or magnetic resonance imaging (MRI) of the brain should be performed. The choice of study depends on how easy the study is to obtain and whether structural or vascular causes can be ruled out clinically. Other studies to consider, depending on the clinical presentation, include chest radiograph (evaluates for pneumonia), electrocardiograph (ECG) (excludes myocardial infarction or arrhythmia), electroencephalograph (EEG), and lumbar puncture, especially if there is concern for CNS infection.
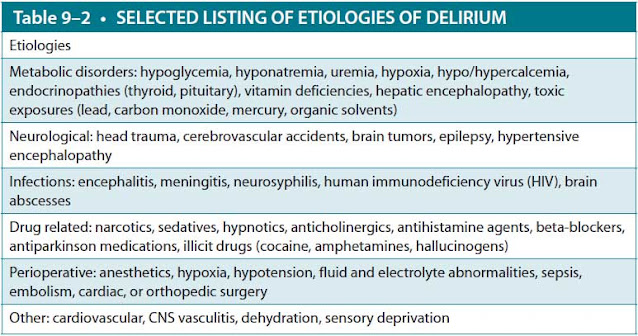
The differential diagnosis for delirium is extensive (Table 9–2) and includes metabolic causes, infections, drug-related causes, primary neurologic abnormalities, trauma, and perioperative causes. Importantly, delirium must be differentiated from dementia. Typically, demented patients have a history of chronic (>6 months) progression with normal attention (except in advanced cases) and level of consciousness. Perceptual disturbances and a fluctuating course are less common with dementia.
Treatment
The treatment is dependent on the etiology of delirium, with the use of drug-related treatments being directed toward symptoms such as agitation, hallucinations, and paranoia. The most common medications used include the neuroleptics such as haloperidol (Haldol), quetiapine (Seroquel), risperidone (Risperdal), and rarely benzodiazepines. These medications should be used judiciously and only when absolutely necessary, especially in the geriatric population. Nonpharmacologic measures, such as optimizing the sleep–wake cycle with lights on during the day and off at night, minimizing unnecessary stimulation, introducing familiar faces and objects, and keeping a routine, should be employed prior to initiating medications if possible. Elderly patients who are hospitalized, particularly in the ICU setting, often become disoriented and are prone to delirium.
CASE CORRELATION
- See also Case 10 (Concussion), Case 20 (Alzheimer Dementia) and Case 21 (Lewy Body Dementia)
COMPREHENSION QUESTIONS
9.1 An 82-year-old man presents to the emergency room with acute disorientation, hallucinations, and agitation. He had been healthy until last year when he developed diabetes mellitus and suffered a myocardial infarction. His examination is normal except for the symptoms mentioned above. Which of the following is the best next step?
A. Obtain a stat CT scan of the head followed by a lumbar puncture.
B. Review his medication list and talk to family about his recent cognitive state.
C. Obtain a CBC, comprehensive metabolic panel, and urinalysis.
D. Begin treatment with risperidone.
9.2 A 21-year-old man is brought in by emergency medical services (EMS) to the emergency room with agitation, disorientation, hyperalertness, and recent personality changes. He is not known to have any medical problems and had been doing well until yesterday after attending a fraternity party. No one else is known to be ill, and he has not had fever or complained of headache or other symptoms. His examination is unremarkable except for a mildly elevated blood pressure of 146/90 mm Hg. What is the most likely diagnosis?
A. Bacterial meningitis
B. Brain tumor
C. Cerebrovascular accident
D. Hallucinogen use
9.3 A 65-year-old man is admitted to the ICU with an acute change in mental status. Which of the following features is more likely to be delirium versus dementia?
A. Chronic loss of recent memory
B. Loss of cognitive ability
C. Fluctuating level of attention
D. History of head trauma
ANSWERS
9.1 B. History is key in trying to determine the etiology of delirium, so obtaining further information from caregivers or family including reviewing his medication list is critical. It is possible that his symptoms are caused by medications he is taking or that he has suffered another myocardial infarction and complained of chest pain before having an alteration in mental status. Obtaining a CBC, comprehensive metabolic panel, and urinalysis are important and will need to be performed, but they are not the next step in this patient’s evaluation.
9.2 D. The most likely culprit of his delirium is hallucinogen use, as he is in an age group at risk for this. He does not have fever or meningismus to suggest bacterial meningitis, and the lack of focal findings on examination argues against a brain tumor or stroke.
9.3 C. Typically, demented patients have a history of chronic (>6 months) progression with normal attention (except advanced cases) and level of consciousness. Perceptual disturbances and fluctuating course are less common with dementia. Up to 40% of ICU patients develop delirium. About 25% of patients admitted for delirium will die. Fluctuation of level of attention is the distinguishing feature of delirium.
CLINICAL PEARLS
|
▶ Delirium is differentiated from
dementia in that delirium involves acute changes in mentation with
fluctuating altered levels of consciousness and attention.
▶ Delirium has a myriad of etiologies
including toxins, medications (illicit and nonillicit), electrolyte or
acid/base disturbances, and infections such as urinary tract infections or
pneumonia.
▶ Delirium often lasts only
approximately 1 week, although it can take several weeks for cognitive function
to return to normal levels. Full recovery is common.
▶ The history and physical examination
are the most important tools in evaluating delirium.
|
REFERENCES
Chan D, Brennan NJ. Delirium: making the diagnosis, improving the prognosis. Geriatrics. 1999; 54(3):28-30, 36, 39-42.
Mendez AM. Delirium. In: Bradley WG, Daroff, RB, Fenichel G, Jankovic J, eds. Neurology in Clinical Practice. 4th ed. Philadelphia, PA: Butterworth-Heinemann; 2003.
Patidar KR, Bajaj JS. Covert and overt hepatic encephalopathy: diagnosis and management. Clin Gastroenterol Hepatol. 2015;13(12):2048-2061.
Sipahimalani A, Masand PS. Use of risperidone in delirium: case reports. Ann Clin Psychiat. 1997;9(2): 105-107.
Wilber ST, Ondrejka JE. Altered mental status and delerium. Emerg Med Clin North Am. 2016;34(3): 649-665.


0 comments:
Post a Comment
Note: Only a member of this blog may post a comment.