Hemoptysis/Lung Cancer Case File
Eugene C. Toy, MD, Gabriel M. Aisenberg, MD
Case 18
A 68-year-old woman is brought to the emergency center after coughing up several tablespoons of bright red blood. For the previous 3 to 4 months, she has had a chronic nonproductive cough but no fevers. More recently, she has noticed some scant blood-streaked sputum. She also reports increased fatigue, decreased appetite, and a 25-lb weight loss in the past 3 months. She denies chest pain, fever, chills, or night sweats. The patient drinks two martinis every day and has smoked one pack of cigarettes per day for the past 35 years. Other than alcohol and tobacco use, she has not had any additional medical issues. She worked in a library for 35 years and has no history of occupational exposures. She does not take any medication except for one low-dose aspirin per day.
The patient is a mildly anxious appearing, thin woman who is alert and oriented. Her blood pressure is 150/90 mm Hg, heart rate is 88 beats per minute (bpm), respiratory rate is 16 breaths/min, and temperature is 99.2 °F. Neck examination reveals no lymphadenopathy, thyromegaly, or carotid bruit. The chest has scattered rhonchi bilaterally, with no wheezes or crackles. Cardiovascular examination reveals a regular rate and rhythm, without rubs, gallops, or murmurs. The abdomen is benign with no hepatosplenomegaly. Examination of her extremities reveals no cyanosis; there is finger clubbing. Neurologic examination is normal.
▶ What is your next step?
▶ What is the most likely diagnosis?
▶ What is the major risk factor?
ANSWERS TO CASE 18:
Hemoptysis/Lung Cancer
Summary: A 68-year-old woman presents with
- A history of smoking one pack of cigarettes per day for the past 35 years
- A chronic, nonproductive cough with recent blood-streaked sputum
- Increased fatigability, reduced appetite, and 3 months of unintentional weight loss
- Absence of fever, chills, and night sweats
- Physical examination revealing scattered rhonchi bilaterally and digital clubbing
Next step: Chest imaging, either x-ray or computed tomography (CT) scan.
Most likely diagnosis: Lung cancer is the most likely diagnosis due to the presence of hemoptysis, unintentional weight loss, and clubbing of the fingers in an individual with significant smoking history.
Major risk factor: Smoking, especially for longer than 30 years.
- Describe the differential diagnosis for hemoptysis. (EPA 2, 10)
- Be familiar with the risk factors for and the clinical presentation of lung cancer (including superior vena cava [SVC] syndrome and Horner syndrome). (EPA 1, 3, 12)
- Know the workup of the solitary pulmonary nodule. (EPA 3)
- List the general principles of the treatment of lung cancer. (EPA 4, 9)
Considerations
The most likely diagnosis in this case is lung cancer. On physical examination, there is finger clubbing, which is an enlargement of the terminal digital phalanges with loss of the nail bed angle. In pulmonary disease, clubbing of the fingers is most commonly seen in patients with lung cancer, interstitial pulmonary fibrosis, or chronic septic conditions, such as bronchiectasis or lung abscess. This patient will require imaging studies such as a chest x-ray and likely CT of the chest and, if abnormalities are seen, a biopsy procedure to establish a tissue diagnosis. In the meantime, she will benefit from rest and cough suppression to minimize her hemoptysis, which may be acutely life threatening if massive bleeding occurs. Though it may not affect prognosis, it is advisable that she also stop smoking at this time.
APPROACH TO:
Hemoptysis and Lung Cancer
DEFINITIONS
HORNER SYNDROME: Symptoms are ptosis, loss of pupillary dilation (miosis), and loss of sweating on the ipsilateral side (anhidrosis) caused by compression of the superior cervical ganglion and resultant loss of sympathetic innervation. This is usually related to a superior sulcus tumor.
HEMOPTYSIS: An expectoration of blood from the respiratory tract.
MASSIVE HEMOPTYSIS: A consensus definition has not been established but typically is defined as 250 mL or more of fresh blood coughed up in 24 hours.
SUPERIOR VENA CAVA (SVC) SYNDROME: Obstruction of venous drainage, usually by extrinsic compression of the SVC, leading to edema of the face, neck, and upper part of the torso, and formation of prominent collateral veins on the upper chest.
CLINICAL APPROACH TO HEMOPTYSIS
Pathophysiology
Hemoptysis is an alarming symptom, both because it may be a manifestation of a serious underlying diagnosis, such as malignancy, and because massive hemoptysis itself can be deadly by filling up alveolar air spaces and causing asphyxiation. Hemoptysis, particularly if in large amounts or recurrent, is a potentially fatal event, thus requiring an immediate search for the cause and precise location of the bleeding. Hemoptysis must be differentiated from hematemesis and epistaxis. Currently, the most common causes of hemoptysis in the United States are bronchitis and lung cancer. In prior eras, the most common causes have been tuberculosis, lung abscess, and bronchiectasis. As stated previously, a good history is an important diagnostic step: Blood-streaked purulent sputum suggests bronchitis; chronic copious sputum production suggests bronchiectasis. Hemoptysis with an acute onset of pleuritic chest pain and dyspnea suggests a pulmonary embolism.
Clinical Presentation
History. A targeted history for patients presenting with hemoptysis is an essential diagnostic step, as it may direct the subsequent steps. It is important to discern how much blood has been expectorated in the past 24 hours and how often the hemoptysis as occurred. These questions are essential in evaluating the acuity and severity of the hemoptysis and may prompt additional questions, such as whether the patient’s airway needs to be protected emergently. It is also necessary to probe about a past history of chronic respiratory disease or respiratory problems (chronic obstructive pulmonary disease, cystic fibrosis, chronic bronchitis, interstitial lung fibrosis, recurrent pneumonia). Specific lung diseases may predispose to bronchiectasis and to airway diseases more prone to hemoptysis. Questions regarding an infectious etiology are also imperative. Is the blood mixed with phlegm? Is that sputum clear or purulent? Additionally, fevers, chills, and night sweats may lead to either an infectious or malignant root cause depending on severity and frequency. Smoking history and environmental exposures should also be assessed. These questions should be followed up by asking about degree and duration of exposure.
Physical examination. Examination of a patient can reveal many cues regarding what the underlying diagnosis may be. When presenting with hemoptysis, the lung examination is of particular importance, but additional hints may be supplied by a complete physical examination. Pulmonary examination may reveal rhonchi or low-pitched continuous sounds that suggest secretions in the airway, and/or wheezes or high-pitched continuous sounds with a hissing quality that suggest narrowed airways. Crackles (rales) are considered intermittent discontinuous sounds and may point to several different ailments, such as heart failure, pneumonia, bronchitis, or bronchiectasis. Clubbing of the fingers is defined as enlargement of the terminal digital phalanges with loss of the nail bed angle. In pulmonary disease, clubbing of the fingers is most commonly seen in patients with lung cancer, interstitial pulmonary fibrosis, or chronic septic conditions, such as bronchiectasis or lung abscess.
Laboratory Tests/Imaging. Every patient with hemoptysis should undergo a chest x-ray or CT to look for a mass lesion, evidence of bronchiectasis, or parenchymal lung disease. If the chest imaging reveals a lung mass, the patient should undergo fiber-optic bronchoscopy to localize the site of bleeding and to visualize and attempt to biopsy any endobronchial lesion.
Treatment
Patients with massive hemoptysis require urgent measures to maintain their airway and to prevent spilling of blood into unaffected areas of the lungs. These patients should be kept at rest with cough suppressants. If the bleeding is localized to one lung, the affected side should be placed in a dependent position so that bleeding does not flow into the contralateral side. They may also require endotracheal intubation and rigid bronchoscopy for better airway control and suction capacity. Urgent referral to interventional radiology for bronchial artery embolization or thoracic surgery for resection may also be required if bleeding is not amenable to bronchoscopic intervention.
CLINICAL APPROACH TO LUNG CANCER
Pathophysiology
Primary lung cancer, or bronchogenic carcinoma, is the leading cause of cancer deaths in both men and women. Approximately 85% of lung cancers of all cell types are linked to smoking. Of the 15% of lung cancers that are not related to smoking, the majority are found in women for reasons that are unknown. Thoracic radiation exposure and exposure to occupational or environmental toxins, such as asbestos or radon, are also associated with increased risk of developing lung cancer.
Data from the National Lung Screening Trial demonstrated a reduction in lung cancer mortality in select high-risk patients who undergo an annual low-dose CT scan of the chest; these high-risk patients include adults 55 to 80 years old with a 30 pack-year smoking history who are current smokers, or quit within the last 15 years, and do not have other life-limiting diseases.
Clinical Presentation
Only 5% to 15% of patients with lung cancer are asymptomatic when diagnosed. In these cases, a lung nodule usually is found incidentally on chest x-ray or CT.
Endobronchial tumors may present with cough or with hemoptysis. Chest pain is also a possible symptom of lung cancer and suggests pleural involvement or neoplastic invasion of the chest wall. Constitutional symptoms like weight loss, malaise, and fatigue usually develop later in the disease course. Malignant pleural effusion is common and may lead to presenting symptoms of shortness of breath and chest pain. Two well-known syndromes are associated with lung cancer: Horner syndrome and SVC syndrome. Horner syndrome is caused by the invasion of the cervicothoracic sympathetic nerves and occurs with apical tumors (Pancoast tumor). Phrenic nerve invasion may cause diaphragmatic paralysis. SVC obstruction is produced by direct extension of the tumor or by compression from the neighboring lymph nodes. SVC syndrome has a dramatic clinical presentation and is a medical emergency requiring urgent care. The clinical presentation is facial swelling, hoarseness of voice, arm swelling, stridor, and nasal stuffiness.
Once a patient presents with symptoms or radiographic findings suggestive of lung cancer, the next steps are as follows:
- Tissue diagnosis to establish malignant diagnosis and histologic type
- Staging to determine resectability or curative potential
- Cancer treatment: surgery, radiotherapy, traditional chemotherapy, or targeted therapies
Classification. Histologically, primary lung cancer can be divided into two major categories with important therapeutic implications: small cell lung cancer (SCLC) and non–small cell lung cancer (NSCLC). NSCLC accounts for approximately 86% of all primary lung cancers compared to only 14% for SCLC. NSCLC is further classified into three or more major histologic types, including squamous cell carcinoma (SCC), adenocarcinoma, large-cell carcinoma, and others.
SCC usually does not metastasize early. It is usually a central/hilar lesion with local extension that may present with symptoms caused by bronchial obstruction, such as atelectasis and pneumonia. SCC is the most likely lung cancer to cavitate and may be seen on x-ray as a central cavitary lesion. It may also produce parathyroid hormone–related protein, which causes hypercalcemia.
Adenocarcinoma and large-cell cancer are peripheral lesions. Adenocarcinoma metastasizes early, especially to the central nervous system (CNS), bones, and adrenal glands. Adenocarcinoma has the lowest association with smoking and a stronger association with pulmonary scars/fibrosis. Large-cell cancer is usually a peripheral lesion and tends to metastasize to the CNS and mediastinum. It can cause SVC
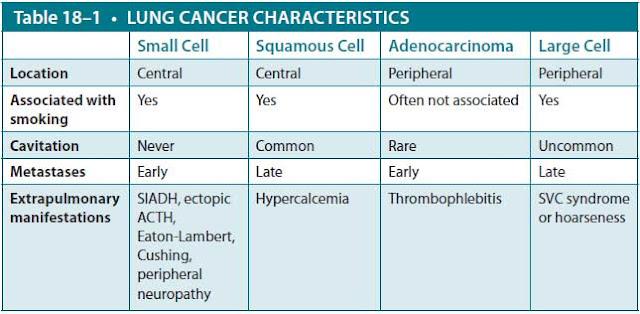
Abbreviations: ACTH, corticotropin (adrenocorticotropic hormone); SIADH, syndrome of inappropriate secretion of antidiuretic hormone; SVC, superior vena cava.
syndrome or hoarseness as a consequence of laryngeal nerve paralysis. Individually, the other NSCLC subtypes represent only a fraction of total lung cancer cases and have a varied presentation.
Small-cell carcinoma is made up of poorly differentiated neuroendocrine cells. It is extremely aggressive but in general responds better to chemotherapy than NSCLC. The primary lesion is typically central. Eighty percent of patients have metastasis at the time of diagnosis, so its treatment generally differs from that of other lung cancers. Contrary to other lung cancers, cavitation never occurs in small-cell cancer. SCLC can cause paraneoplastic syndromes, including syndrome of inappropriate secretion of antidiuretic hormone (SIADH), ectopic adrenocorticotropic hormone (ACTH; corticotropin) production, and Lambert-Eaton syndrome. Table 18–1 lists typical characteristics of various cell types.
SCLC is initially very responsive to chemotherapy and radiation therapy, but unfortunately, most SCLC relapses. Additionally, SCLC has almost always spread at time of diagnosis, so surgical treatment with curative intent is not possible. In contrast, NSCLC is much less responsive to chemotherapy or to radiation, but tumors that are localized at time of diagnosis may be treated with curative surgery or with radiation therapy. The majority of NSCLC subtypes have similar treatment and prognoses at similar stages.
Treatment
Treatment of lung cancer consists of surgical resection, chemotherapy, and/or radiation therapy in different combinations, depending on the tissue type and extent of the disease, and may be performed with either curative or palliative intent. Targeted therapies against mutations prevalent in adenocarcinoma subtypes are increasingly being used with variable success.
Once the diagnosis of NSCLC is made, the next step is to stage the disease to decide whether the cancer is resectable and thus potentially curable. Patients may be candidates for resection if the cancer is localized to one hemithorax, which may include ipsilateral, but not contralateral, hilar and mediastinal lymph nodes, and there are no major anatomic barriers to successful resection.
SCLC is nearly always metastatic at time of diagnosis and, therefore, not eligible for surgical resection. It is staged as either limited, disease confined to one hemithorax that can be treated within a radiotherapy port, or extensive, disease with contralateral lung involvement or distant metastases that is treated with systemic therapies. Patients with untreated, advanced SCLC have a poor prognosis, with survival generally measured in weeks. Approximately 20% to 30% of patients with limited-stage disease can be cured with radiotherapy and chemotherapy; however, the prognosis for relapsed patients is poor.
Because most lung cancer occurs in older patients who have been smokers, patients with lung cancer frequently have underlying cardiopulmonary disease and require preoperative evaluation, including pulmonary function testing, to predict whether they have sufficient pulmonary reserve to tolerate a lobectomy (removal of one lung lobe) or pneumonectomy (removal of one lung). Performance status, or general well-being of the patient, is also taken into consideration when deciding if a patient is even a candidate for therapy or what type of therapy is appropriate.
Solitary Pulmonary Nodule. The solitary pulmonary nodule is defined as a nodule surrounded by normal parenchyma. Most incidentally discovered nodules are benign, but differentiation between benign etiologies and early-stage malignancy can be challenging. Proper management of a solitary nodule in an individual patient depends on a variety of elements: age, risk factors, presence of calcifications, and size of the nodule. Of these factors, size is highly predictive. Larger lesions are more likely to be malignant than smaller lesions. In one study, the likelihood of malignancy was 0.2% for nodules smaller than 3 mm, 0.9% for nodules 4 to 7 mm, 18% for nodules 8 to 20 mm, and 50% for nodules larger than 20 mm. Put another way, greater than 99% of nodules measuring less than 8 mm are benign.
The presence and type of calcification on a solitary pulmonary nodule can be helpful. “Popcorn” and “bull’s-eye” calcifications suggest a benign process, whereas absence of calcification increases the likelihood of malignancy.
Professional organizations such as the Fleischner Society offer a widely accepted algorithm for follow-up imaging of solitary pulmonary nodules. Generally speaking, for lesions 8 mm or less, serial CT imaging is an acceptable strategy to monitor for growth. Radiographic stability for 2 years or longer is strong evidence of benign etiology. For lesions 1 cm or greater, additional studies, such as positron emission tomography scan, transthoracic needle biopsy, or bronchoscopic evaluation, may be indicated.
CASE CORRELATION
- See also Case 15 (Chronic Obstructive Pulmonary Disease), Case 16 (Chronic Cough/Asthma), Case 17 (Pleural Effusion, Parapneumonic), and Case 19 (Community-Acquired Pneumonia).
COMPREHENSION QUESTIONS
18.1 A 67-year-old man presents to the office with a 3-day history of headaches and progressive swelling of his face and right arm. He has a 50 pack-year smoking history and was diagnosed with chronic obstructive pulmonary disease 15 years ago. On examination, he is found to have redness and edema of his face and his right arm, which is of recent onset. Which of the following is the most likely diagnosis?
A. Angioedema
B. Hypothyroidism
C. Superior vena cava syndrome
D. Trichinosis
18.2 A 64-year-old woman is being seen in the office complaining of a hoarse voice for 4 months. She denies fever, sore throat, or cough. On examination, her respiratory rate is 26 breaths/min, temperature is 98 °F, and heart rate is 100 bpm. She has expiratory wheezes in her left midlung fields bilaterally. Which of the following is the best next step the management of this patient?
A. Prescribe antibiotics for bronchitis.
B. Order a chest x-ray.
C. Advise gargling with saltwater solution.
D. Prescribe an albuterol inhaler.
18.3 A 33-year-old woman is being seen in the office for a dry cough that has persisted for 3 months. She has lost 30 lb without intention over the past 3 months. On examination, she is noted to be cachectic. Examination shows clear lung fields. A chest x-ray shows a 3-cm lung mass. Bronchoscopic biopsy is performed. Which of the following lung cancers is the most likely cell type?
A. Squamous cell
B. Adenocarcinoma
C. Small cell
D. Large cell
18.4 A 52-year-old previously healthy man presents to the emergency center with progressively worsening dyspnea over the past 2 months. Examination shows decreased breath sounds on the right lung zone and dullness on percussion on that side. Chest x-ray shows a 4-cm hilar mass and a large ipsilateral right pleural effusion. Which of the following is the best next step in the management of this patient?
A. CT scan of the chest, head, and abdomen for cancer staging.
B. Pulmonary function testing to evaluate pulmonary reserve to evaluate for pulmonectomy.
C. Biopsy and pathologic evaluation of the hilar mass.
D. Initiate palliative radiation because the patient is not a candidate for curative resection.
ANSWERS
18.1 C. The patient has features of SVC syndrome, caused by compression of the SVC, almost always by a thoracic malignancy. Urgent diagnosis and treatment are mandatory because of impaired cerebral venous drainage and resultant increased intracranial pressure or possibly fatal intracranial venous thrombosis. Angioedema (answer A), hypothyroidism (answer B), and trichinosis (answer D) all may cause facial swelling, but not the redness (plethora) or swelling of the arm.
18.2 B. This patient has chronic hoarseness and unilateral wheezing. This suggests an intrathoracic mass causing bronchial obstruction and impairment of the recurrent laryngeal nerve, causing vocal cord paralysis. Thus, an imaging study of the chest is essential. If the chest x-ray is negative, the voice hoarseness still needs to be pursued, such as by laryngoscopy, to assess for pathology of the vocal cords or larynx. Answer A (antibiotics for bronchitis) may be appropriate in the clinical setting of 1-2 weeks of cough and voice hoarseness; however, once voice hoarseness has lasted longer 3 weeks, investigation for cancer must be undertaken. Similarly, answer C (Saltwater gargling) and answer D (Albuterol inhaler) are symptomatic measures, and more aggressive diagnostic interventions are required.
18.3 B. The most common form of lung cancer found in nonsmokers, young patients, and women is adenocarcinoma. Of note, 85% of patients with lung cancer of all histologic types have a smoking history.
18.4 C. Biopsy of the hilar mass is important because tissue diagnosis is essential for proper treatment of any malignancy; for this reason, biopsy should generally be the first step. Once a specific tissue diagnosis is obtained, the cancer is staged (answer A) for prognosis and to guide therapy. Therapeutic options may be surgical resection, chemotherapy, or radiotherapy. Questions for this patient include the tissue type, location of spread, and whether the pleural effusion is caused by malignancy. Answer B (Pulmonary function tests) are not indicated until a diagnosis is determined to see what treatment is needed. Answer D (Palliative radiation) is not indicated until cancer is diagnosed.
CLINICAL PEARLS
▶ Most patients with hemoptysis require evaluation with bronchoscopy. Massive hemoptysis may result in death by asphyxiation.
▶Lung cancer is the leading cause of cancer deaths in men and women.
▶A solitary pulmonary nodule measuring 8 mm or less can be followed radiographically. For larger lesions, a biopsy, whether bronchoscopic, percutaneous, or surgical, should be considered.
▶Steps in management of a patient with suspected lung cancer include tissue diagnosis, staging, preoperative evaluation, and treatment with surgery, radiotherapy, or chemotherapy.
▶Small cell lung cancer usually is metastatic at the time of diagnosis and not resectable. NSCLC may be curable by resection if it is early stage and the patient has sufficient pulmonary reserve.
REFERENCES
Aberle DR, Adams AM, Berg CD, et al. Reduced lung-cancer mortality with low-dose computed tomographic screening. N Engl J Med. 2011;365(5):395-409.
Eddy JB. Clinical assessment and management of massive hemoptysis. Crit Care Med. 2000;28(5):1642-1647.
Horn L, Pao W, Johnson DH. Neoplasms of the lung. In: Jameson JL, Fauci AS, Kasper DL, et al, eds. Harrison’s Principles of Internal Medicine. 20th ed. New York, NY: McGraw Hill; 2018:737-753.
Kritek P, Fanta C. Cough and hemoptysis. In: Jameson JL, Fauci AS, Kasper DL, et al, eds. Harrison’s Principles of Internal Medicine. 20th ed. New York, NY: McGraw Hill; 2012:2170-2177.
Libby DM, Smith JP, Altorki NK, et al. Managing the small pulmonary nodule discovered by CT. Chest. 2004;125:1522-1529.

0 comments:
Post a Comment
Note: Only a member of this blog may post a comment.