Ptosis (Myasthenia Gravis) Case File
Eugene C. Toy, MD, Ericka Simpson, MD, Pedro Mancias, MD, Erin E. Furr-Stimming, MD
CASE 36
A 30-year-old woman presents with a 1-month history of intermittent ptosis (droopiness of the eyelids) and fatigue. She is a surgery resident and has been on call every third night over the past 2 months and has been attributing her fatigue to her hectic call schedule. However, she became concerned when she acutely developed ptosis last month after an exhausting night on call. The next morning after sufficient rest, her ptosis had resolved. Since her first episode, she has experienced three more episodes of ptosis over the past month. They all have occurred while she has been postcall or fatigued and have improved by the morning. Her children have pointed out to her that she can’t keep up with them when they’re riding their bicycles. Today, she developed ptosis while assisting in a complicated abdominal surgery. Her attending asked her to scrub out of the surgery and immediately seek medical evaluation. She has not experienced diplopia, dysarthria, dysphagia, difficulty walking up the stairs, difficulty blowdrying her hair, or shortness of breath. She has no other medical issues.
Her neurologic examination is notable for normal mental status and speech. Her cranial nerve examination reveals bilateral ptosis on primary gaze, which worsens with sustained upward gaze for 90 seconds. Extraocular muscles are intact, as is her facial strength. Her motor strength is normal with the exception of 4+/5 in the deltoid muscles bilaterally. On repetitive testing of the right iliopsoas muscle, fatigability is elicited, which improves after 2 minutes of rest. Her sensory examination and deep tendon reflexes (DTRs) are normal.
▶ What is the most likely diagnosis?
▶ What is the best test to confirm the diagnosis?
▶ What is the next step in therapy?
ANSWERS TO CASE 36:
Ptosis (Myasthenia Gravis)
Summary: A 30-year-old woman with no significant medical history presents with a 2-month history of fatigue and a 1-month history of intermittent ptosis. She does not complain of proximal muscle weakness, dysarthria, shortness of breath, or dysphagia. Her examination is notable for ptosis on primary gaze, which worsens with sustained upward gaze, weakness of the deltoid muscles, and fatigability of the iliopsoas muscle, which improves with rest.
- Most likely diagnosis: Myasthenia gravis
- Best confirmatory test: Antiacetylcholine (anti-ACh) receptor antibodies
- Next step in therapy: Acetylcholinesterase inhibitors (pyridostigmine) and immunosuppression
- Know a diagnostic approach to ptosis and understand how associated symptoms are helpful in determining the etiology.
- Be familiar with the differential diagnosis of ptosis.
- Understand the basic pathophysiology of myasthenia gravis and the rationale for treatment.
Considerations
This 30-year-old woman developed fatigue and ptosis over a short period of time. The most concerning symptom is ptosis, as it has already interfered with her ability to perform her duties as a resident. In this particular case, the patient complained only of fatigue in addition to the ptosis, but findings on examination show fatigability and proximal muscle weakness. Based on this, the cause of ptosis can be pinpointed to either a neuromuscular junction transmission disorder or myopathy. Electromyography (EMG)/nerve conduction study (NCS) can help differentiate between the two, and if indicative of a neuromuscular junction issue, then the diagnosis of myasthenia gravis is most likely. Forced vital capacity and negative inspiratory force are very important in evaluating patients with suspected neuromuscular disease associated with diaphragmatic weakness. In this particular case, the patient does not complain of shortness of breath; however, the history of fatigue and having difficulty keeping up with her children while bike riding should raise the concern. Forced vital capacity and negative inspiratory force are simple bedside tests that can provide further information on the respiratory status of an individual.
DEFINITIONS
ANTI-MUSK ANTIBODIES: Muscle-specific receptor tyrosine kinase (MuSK) antibodies. MuSK is a surface membrane enzyme that is critical for aggregating ACh receptors during neuromuscular junction development. It is seen in approximately 40% of myasthenics who are seronegative for ACh receptor antibodies.
BULBAR WEAKNESS: Weakness in muscle groups innervated by cranial nerves IX, X, XI, and XII that most often results in dysphagia, dysphonia, dysarthria, and slurring of speech.
ANTI-Lrp4 ANTIBODIES: Low-density lipoprotein receptor–related protein 4 (Lrp4) antibodies. Lrp4 is a protein that binds to MuSK, which is critical for the aggregation of ACh receptors and neuromuscular junction development. Anti-Lrp4 antibodies are seen in some double-seronegative (patients without anti-MuSK or anti-ACh antibodies) myasthenic patients.
MYOPATHIC: A disorder of muscle or muscle tissue.
NEUROPATHIC: A disorder affecting the anterior horn cell, nerve root, plexus, or peripheral nerves.
CLINICAL APPROACH
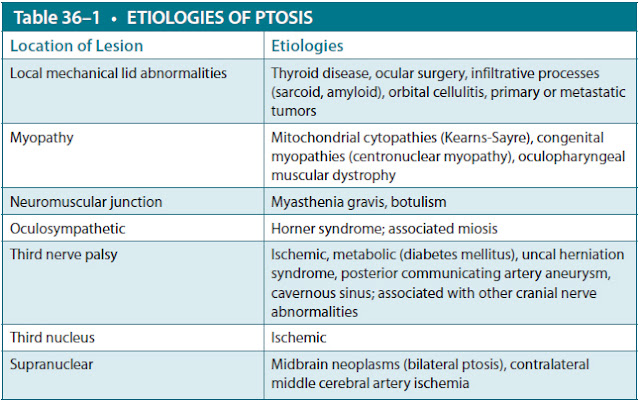
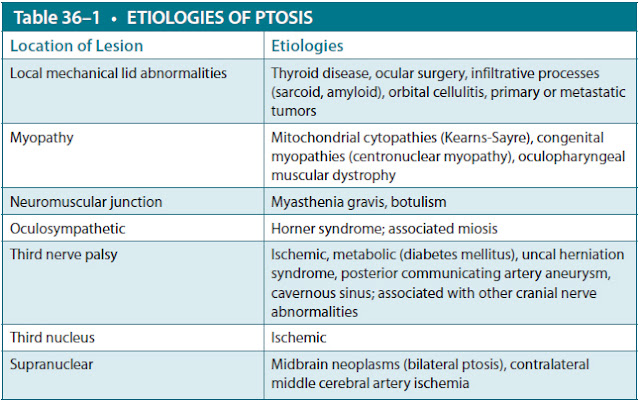
Ptosis is associated with multiple conditions. As noted in Table 36–1, the differential diagnosis will be based on the patient’s symptoms and the clinical findings. Ptosis results from weakness of the levator palpebrae superioris muscle and can occur unilaterally or bilaterally. It becomes evident when the eyelid partially or completely covers the pupil, iris, or other parts of the eye. In some instances, the upper eyelid may only cover the entire pupil, resulting in impaired vision. Acquired ptosis is a sign of an underlying neurologic problem that requires urgent medical evaluation.
The possible etiologies of ptosis include local mechanical lid abnormalities, myopathy, diseases of the neuromuscular junction such as myasthenia gravis, oculosympathetic lesions, third nuclear pathology, and supranuclear lesions in the contralateral hemisphere along the territory of the middle cerebral artery.
Associated clinical findings such as miosis, hemiparesis, or other cranial nerve abnormalities will indicate if this is a supranuclear problem, nuclear problem, oculosympathetic problem, third nerve dysfunction, neuromuscular junction transmission disorder, myopathic disorder, or local infiltrative process.
The associated symptoms and findings on neurologic examination are critical to establish the cause of ptosis. Isolated ptosis without other symptoms suggests local mechanical factors as a cause. Conversely, ptosis along with proximal muscle weakness (difficulty climbing up stairs, difficulty arising from a chair, difficulty blow-drying hair, difficulty reaching over the head) suggests an underlying myopathy. Fatigability of muscle (repetitive use of the same muscle leading to loss of strength) with improvement after a short period of rest associated with ptosis suggests an underlying neuromuscular junction transmission disorder. Contralateral hemiparesis or hemitremor accompanying ptosis suggests ischemic lesions in the midbrain affecting the third nerve. Ptosis from a third nerve palsy associated with other cranial nerve dysfunction such as IV, V, and VI is seen with cavernous sinus syndrome. The history and clinical examination are key to evaluate patients with ptosis. In this particular case, the patient gives a history of fatigue and ptosis, and her examination is also notable for proximal muscle weakness and fatigability. These features are suggestive of an underlying neuromuscular junction transmission disorder or, less likely, a myopathy.
The evaluation of a patient with ptosis should be guided by associated symptoms and findings on clinical examination. Serologic studies consisting of a comprehensive metabolic panel and complete blood count (CBC) with differential are helpful in ascertaining metabolic processes such as diabetes mellitus, hypokalemia, infections, or even malignancies. A vasculitis screen with antinuclear antibody (ANA) and erythrocyte sedimentation rate (ESR) can be helpful in evaluating for inflammatory processes such as systemic lupus erythematosus. Thyroid function studies evaluate for thyroid disease. Serum creatine phosphokinase (CPK) is helpful in evaluating for myopathies. Serum lactate can be helpful in screening for mitochondrial cytopathies. Specifically, ACh receptor antibodies are used to evaluate for myasthenia gravis.
If there is evidence of multiple cranial nerve involvement or of contralateral hemiparesis on physical examination, magnetic resonance imaging (MRI) of the brain should be obtained, as these findings are suggestive of cavernous sinus or brainstem pathology. If ptosis is associated with an isolated third nerve palsy, both an MRI of the brain and magnetic resonance angiogram (MRA) should be obtained, as this may suggest a possible posterior communicating artery aneurysm.
An EMG/NCS is one of the most important studies in evaluating patients with suspected neuromuscular diseases. It can be helpful in differentiating between a neuropathic process, myopathic process, and disorder of the neuromuscular junction. Additionally, it provides information as to the severity and chronicity of the process. It is a two-part study consisting of NCS and EMG. NCSs evaluate conduction velocity of a nerve between two different points. It evaluates both motor and sensory nerves. Repetitive nerve stimulation uses a 2- to 5-Hz train of stimulations to a nerve innervating a symptomatic muscle. An amplitude decrement of 10% or greater between the first and fourth stimulations is suggestive of a postsynaptic neuromuscular junction defect. Repetitive nerve stimulation studies are done before and after brief exercise and then repeated after 5 minutes of rest. EMG evaluates the electrical properties of the muscle at rest and on contraction, and can help distinguish a myopathy from a neuropathy.
MYASTHENIA GRAVIS
Myasthenia gravis is an uncommon autoimmune disorder affecting the neuromuscular junction postsynaptically. It is characterized by skeletal muscle weakness and fatigability. The prevalence of myasthenia gravis in the United States is approximately 14.2 cases per 100,000. It is estimated that the annual incidence of myasthenia gravis in United States is 2:1,000,000. Women are affected more than men at a ratio of 3:2. Although myasthenia gravis can occur at any age, it tends to peak in females during the second and third decades of life and in males during the sixth and seventh decade of life. Women have also been noted to have a second peak during their eighth decade of life.
The classic symptoms are those of skeletal muscle weakness affecting the ocular, facial, bulbar, respiratory, and limb muscles. The weakness quickly fluctuates and worsens throughout the day. Importantly, there is fatigability of the muscles with recovery to baseline strength after a short period of rest. Approximately 75% of patients will present with ocular disturbances including ptosis and diplopia. Up to 90% of patients with myasthenia gravis will eventually experience ocular symptoms. Ptosis can be bilateral or unilateral and can shift quickly from one eye to the other. Weakness of the extraocular muscles causing diplopia can be asymmetrical.
Other common complaints include dysphagia, dysarthria, shortness of breath, fatigue with chewing, difficulty holding the head up, limb weakness, and torso weakness. Limb weakness is most commonly proximal and typically presents as difficulty raising the arms above the head, climbing up the stairs, or rising from a chair. Commonly affected muscles include the neck flexors, deltoids, triceps, finger extensors, wrist extensors, hip flexors, and foot dorsiflexors. Fatigability of these muscles is frequently observed on physical examination.
Weakness of the pharyngeal and tongue muscles results in impaired speech and swallowing. Speech can have a nasal quality to it or be slurred. This is most noticeable when the patient continues to talk for prolonged periods of time. A snarling expression on attempted smile can be present, which denotes facial weakness. Additionally, weakness of the orbicularis oculi muscles can be present on examination when the eyelids are separated against forced eye closure. Patients do not often complain of facial weakness.
Shortness of breath results from weakness of the intercostal and diaphragm muscles. This can become a medical emergency requiring emergent intubation. A good way of evaluating the status of respiratory muscle weakness is to perform a forced vital capacity and negative inspiratory force, as these studies can reflect neuromuscular respiratory fatigue before changes in oxygen saturation. Therefore, significant precautions should be undertaken when patients are evaluated in the emergency room, as they can decompensate very quickly and require immediate intubation.
Physiology of Myasthenia Gravis
Normally, an excitatory postsynaptic end-plate potential is generated at the neuromuscular junction when ACh is released into the synaptic cleft and diffuses to the postsynaptic membrane to bind to nicotinic ACh receptors. Once the threshold for depolarization is reached, an action potential will be generated that spreads across the muscle, leading to contraction. ACh is then removed from the synaptic cleft by acetylcholinesterase or via presynaptic membrane reuptake.
In myasthenia gravis, an action potential is not generated at the postsynaptic membrane (neuromuscular transmission failure), which results in weakness. Failure to generate an action potential is caused by the inability of excitatory postsynaptic end-plate potentials to reach the threshold for depolarization. This is caused by a diminished amount and availability of postsynaptic receptors. If ACh fails to bind to a sufficient number of postsynaptic ACh receptors, the end-plate potentials generated are not enough to reach threshold for depolarization. This, in essence, fails to generate an action potential and thus prevents muscle contraction and causes weakness. Circulating antibodies (ACh receptor antibodies) bind to the ACh receptor and prevent ACh from binding. This in turn allows for cross-linking of receptors, which leads to degradation and eventually receptor internalization. Postsynaptic membrane damage can also occur via complement activation. The number of ACh receptors diminishes over time because of these changes (Figure 36–1).
Diagnostic Testing for Myasthenia Gravis
Laboratory studies for ACh receptor antibodies are the most specific and sensitive test for myasthenia gravis. There are three antibodies described against the ACh receptor: binding (most commonly tested), blocking, and modulating antibodies. Up to 90% of patients with generalized myasthenia gravis (affecting more than the ocular muscles) will have a positive test for one of these antibodies. However, patients with no ACh receptor antibodies can have anti-MuSK antibodies, which have also been associated with myasthenia gravis. In addition, thyroid function studies should always be performed, as concomitant thyroid disease is often seen in myasthenia gravis.
The Tensilon (edrophonium bromide) test has historically been described as the classic diagnostic test. Edrophonium bromide is an acetylcholinesterase inhibitor that rapidly and transiently blocks degradation of ACh, allowing for prolonged stimulation of the muscle and temporary improvement of ptosis. However, edrophonium bromide may not be available in some hospital or clinic settings and requires electrocardiogram (ECG) monitoring during testing for drug-related bradycardia. Another simple bedside test that can be used in patients with ptosis is the ice test. Ice is placed over the ptotic eyelid for 2 minutes. If the ptosis improves after removing the ice, a diagnosis of an underlying neuromuscular junction transmission disorder (ie, myasthenia gravis) can be made. Cooling improves neuromuscular junction transmission, whereas heat worsens it. This is the reason that many patients with myasthenia gravis typically worsen during the summer months.

Figure 36–1. Diagrams of (A) normal and (B) myasthenic neuromuscular junctions. V, vesicles of acetylcholine; M, mitochondria; AChR, Acetylcholine receptor; AChE, Acetylcholine esterase. (Reproduced, with permission, from Kasper DL, et al. Harrison’s Principles of Internal Medicine. 16th ed. New York, NY: McGraw-Hill; 2004:2519.)
Electrodiagnostic studies with EMG/NCS can be performed to evaluate patients with myasthenia gravis. Classically, NCSs are normal. EMG can be normal or can show myopathic features. A more specialized study, single-fiber EMG, is the most sensitive test available for myasthenia gravis; however, it is not very specific and can be abnormal in other neurologic disease states such as neuropathies, amyotrophic lateral sclerosis, and muscular dystrophy.
A computed tomography (CT) scan or MRI of the mediastinum should be performed to exclude thymic enlargement or more importantly, a thymoma. Thymectomy should always be performed in those individuals who have thymoma. An international randomized study of thymectomy in myasthenia gravis was recently completed and showed that in patients receiving a thymectomy, those patients required less steroid therapy at study completion compared to non surgical patients.
Treatment of Myasthenia Gravis
Immunosuppressive agents are the mainstay of treatment for myasthenia gravis. These include corticosteroids, cyclosporine, azathioprine, mycophenolate mofetil, intravenous immunoglobulin, and plasmapheresis. There is no general agreement among experts regarding the timing or use of the other immunosuppressive treatments. Acetylcholinesterase inhibitors such as pyridostigmine only treat the symptoms and not the disease. However, these are routinely used in patients with myasthenia gravis, especially if the only symptoms are ocular.
CASE CORRELATION
- See Case 35 (Facial Paralysis)
COMPREHENSION QUESTIONS
36.1 You evaluate a 23-year-old woman with a history of intermittent ptosis and difficulty walking up the stairs that improves with rest. You suspect a neuromuscular junction disorder. Therefore, which of the following would be most characteristic of this disorder?
A. Myotonia and distal muscle weakness
B. Decreased DTRs out of proportion to the degree of muscle weakness
C. Fatigable proximal and symmetric muscle weakness with prominent ocular involvement
D. Fatigable distal and asymmetric muscle weakness with prominent ocular involvement
E. Ptosis, diplopia, and nonreactive pupils
36.2 Which of the following is a critical difference between myogenic processes and disorders of the neuromuscular junction?
A. Fatigability with improvement after rest in neuromuscular junction transmission disorders
B. Weakness of the ocular muscles only in neuromuscular junction transmission disorders
C. Decrement of greater than 5% in myogenic disorders
D. Elevated CPK in neuromuscular junction transmission disorders
E. Right eye ptosis and diplopia and left-sided weakness
36.3 A 52-year-old woman presents with ptosis and ophthalmoplegia. Which study should be performed first?
A. ACh receptor antibodies
B. EMG/NCS
C. Serologic studies for CPK
D. MRI of the brain with MRA
E. Thyroid function studies
36.4 A 62-year-old man with ptosis with an abnormal brain MRI is being monitored in the intensive care unit (ICU). Which of the following conditions is the most likely cause for ptosis?
A. Pituitary necrosis
B. Uncal herniation
C. Central herniation
D. Arteriovenous (AV) malformation
ANSWERS
36.1 C. Myasthenia gravis is characterized by fatigable and symmetric proximal muscle weakness with prominent ocular involvement. If decreased, DTRs are diminished in proportion to the degree of muscle weakness, and the pupils are never involved.
36.2 A. Fatigability of muscles with improvement after rest is a hallmark of neuromuscular junction transmission disorders.
36.3 D. The presence of multiple cranial abnormalities along with ptosis is
suggestive of central nervous system pathology, particularly in the brainstem or cavernous sinus.
36.4 B. Central herniation causes compression of the diencephalon, flattening the midbrain and pons; uncal herniation compresses the third cranial nerve, causing ptosis.
CLINICAL PEARLS
|
▶ The etiology of ptosis is best
determined by recognizing associated symptoms that patients present with and
discerning clinical findings on examination.
▶ Ptosis associated with central
nervous system signs and symptoms mandates an MRI of the brain.
▶ Fatigability of muscle with
improvement after a brief period of rest is seen only with neuromuscular
junction transmission disorders.
▶ Up to 90% of patients with myasthenia
gravis will eventually have ocular symptoms.
▶ Local cooling of the eye can improve
function in a ptotic eyelid, similarly to a Tensilon test, and is a rapid,
simple, and inexpensive test for myasthenia gravis.
|
REFERENCES
Keesey JC. Clinical evaluation and management of myasthenia gravis. Muscle Nerve. 2004;29(4):
484-505.
Mills KR. Specialised electromyography and nerve conduction studies. J Neurol Neurosurg Psychiatry. 2005;76:ii36-ii40.
Newsom-Davis J, Cutter G, Wolfe GI, et al. Status of the thymectomy trial for nonthymomatous myasthenia gravis patients receiving prednisone. Ann N Y Acad Sci. 2008;1132:344-347.
Sanders DB, Wolfe GI, Benatar M, et al. International consensus guidance for management of myasthenia gravis: executive summary. Neurology. 2016;87(4):419-425.
Saperstein DS, Barohn RJ. Management of myasthenia gravis. Semin Neurol. 2004;24(1):41-48.
Zisimopoulou P, Evangelakou P, Tzartos J, et al. A comprehensive analysis of the epidemiology and clinical characteristics of anti-LRP4 in myasthenia gravis. J Autoimmun. 2014;52:139-145.


0 comments:
Post a Comment
Note: Only a member of this blog may post a comment.